Contributing physicians in this story
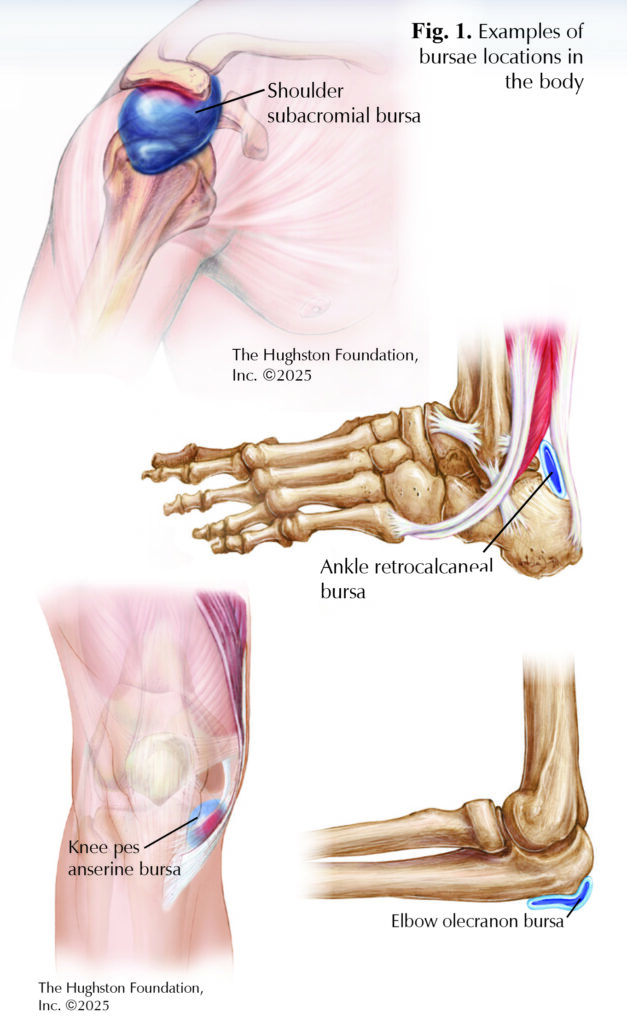 There are approximately 160 bursae throughout your body. A small jelly-like sac, a bursa acts as a cushion to help reduce friction between bones and soft tissue. The submuscular bursae exist between muscles or between muscles and bony prominences. The names of bursae match the location within the human body. Some examples include the shoulder subacromial bursa, ankle retrocalcaneal bursa, knee pes anserine bursa, and the olecranon bursa that is at the tip of the elbow. Bursae of the hip include the ischiogluteal, iliopsoas, and trochanteric. Bursitis develops after friction from a tendon, ligament, or other soft tissue moves over a bony prominence causing the bursa to become inflamed, swollen, and painful. Bursitis can be difficult to live with; but one specific bursa of the hip, once inflamed can cause significant problems.
There are approximately 160 bursae throughout your body. A small jelly-like sac, a bursa acts as a cushion to help reduce friction between bones and soft tissue. The submuscular bursae exist between muscles or between muscles and bony prominences. The names of bursae match the location within the human body. Some examples include the shoulder subacromial bursa, ankle retrocalcaneal bursa, knee pes anserine bursa, and the olecranon bursa that is at the tip of the elbow. Bursae of the hip include the ischiogluteal, iliopsoas, and trochanteric. Bursitis develops after friction from a tendon, ligament, or other soft tissue moves over a bony prominence causing the bursa to become inflamed, swollen, and painful. Bursitis can be difficult to live with; but one specific bursa of the hip, once inflamed can cause significant problems.
Greater trochanteric bursitis and pain syndrome
The name “trochanteric” refers to the upper bony prominence region of the femur (thighbone). The predominant cause of greater trochanteric pain syndrome, trochanteric bursitis, involves inflammation of the bursa between the greater trochanter and the iliotibial band and causes pain on the lateral or outside of the hip. The inflammation often triggered by repetitive stress and trauma, manifests as pain in the lateral thigh after prolonged sitting, stair climbing, or engaging in high-impact exercises.
Greater trochanteric pain syndrome produces hip pain during weightbearing, which can cause fatigue as the day goes on and may disrupt sleep. Inflamed tissue or bursitis is not the only cause of lateral hip pain. Other structures that can cause pain in the region include the gluteus medius tendons and the iliotibial band, which can cause tendonitis, tearing, and even rupture. For this reason, we also refer to lateral hip pain as greater trochanteric pain syndrome, which is a collection of symptoms related to conditions, such as gluteal tears, external snapping hip, and abductor tendinopathy.
Risk Factors
Greater trochanteric pain syndrome typically presents in patients over the age of 45 and is more common in women. Male patients can also experiences the problem, but typically, they are over the age of 65. It is common for the patient to have other associated symptoms including low back, groin, or knee pain. Physicians often find this disease pattern in individuals who do mostly forward-plane activities, such as running or walking, rather than side-to-side activities such as pickle ball, tennis, or racket ball.
Causes
An injury to the hip, knee, or back can cause a change in body mechanics; as a result, the hips take over more weightbearing during walking and performing everyday activities. With weakness in the hip joint, the pelvis cannot maintain being level during walking; therefore, the hip will drop, and the body compensates. This results in the excess friction over the bony trochanteric prominence and thus bursitis. Over time, the gluteus tendons undergoing excessive loads tear or rupture (tear from the bone).
Seeking medical advice
If you continue to experience pain over the lateral side of the hip, and it starts to affect your life, including avoiding certain activities that you otherwise enjoy, then consider seeking advice from an orthopaedist. The initial screening for greater trochanteric pain syndrome begins with x-rays and a physical examination by an orthopaedist. Your doctor may order magnetic resonance imaging, (MRI), an image that shows the bones, muscles, tendons, and ligaments if you experience significant weakness leading to a change in your gait. If symptoms do not improve with a course of physical therapy or home exercises, the orthopaedist can recommend additional treatment options.
Treatment
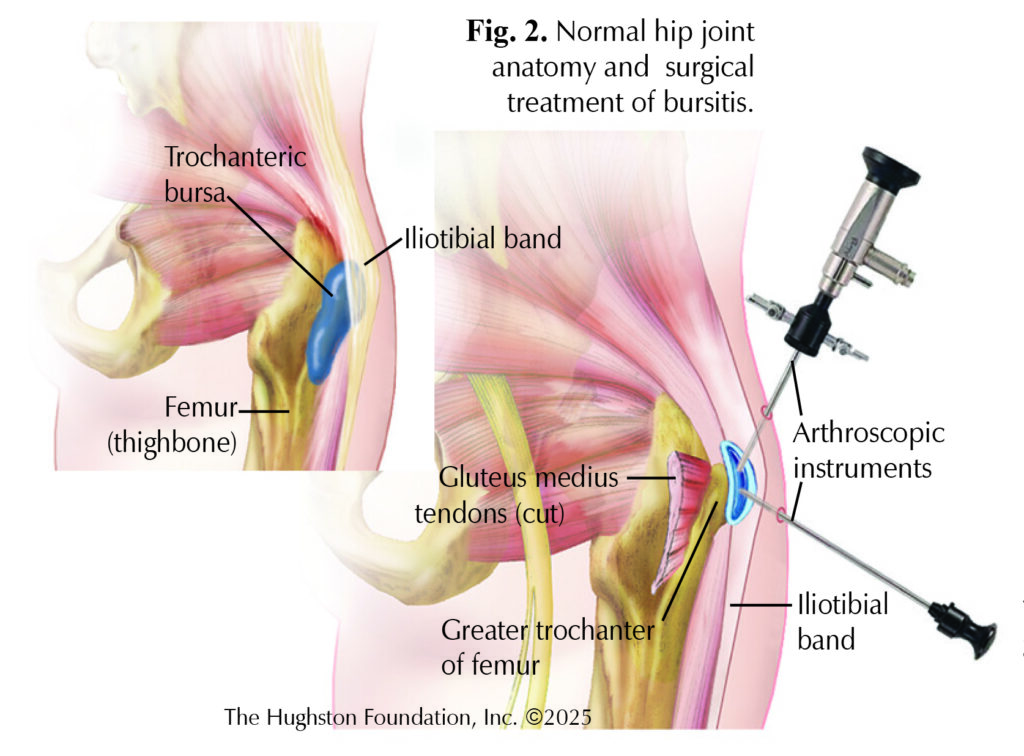 If you do not show weakness during hip testing, your doctor can prescribe conservative treatments, such as physical therapy, a home exercise program, and topical, oral, or injectable anti-inflammatory medications. If surgical intervention is necessary, there are a couple of options depending on the severity of the disease. If you have bursitis without tearing of the tendons, surgical treatment can either be performed using an open technique or arthroscopic (minimally invasive with a camera) surgery. Often, you can return to full activity between 2 to 4 weeks after surgical intervention. If you have bursitis with a partial- or full-thickness tear of the gluteus tendon, you may need a surgical repair procedure. After performing an open or arthroscopic repair, you can expect to return to full activity between 3 to 4 months. Following surgery, your surgeon may prescribe physical therapy that can help to improve your pain and return of hip strength. Persistence in a home exercise program after physical therapy can be key to staying pain free.
If you do not show weakness during hip testing, your doctor can prescribe conservative treatments, such as physical therapy, a home exercise program, and topical, oral, or injectable anti-inflammatory medications. If surgical intervention is necessary, there are a couple of options depending on the severity of the disease. If you have bursitis without tearing of the tendons, surgical treatment can either be performed using an open technique or arthroscopic (minimally invasive with a camera) surgery. Often, you can return to full activity between 2 to 4 weeks after surgical intervention. If you have bursitis with a partial- or full-thickness tear of the gluteus tendon, you may need a surgical repair procedure. After performing an open or arthroscopic repair, you can expect to return to full activity between 3 to 4 months. Following surgery, your surgeon may prescribe physical therapy that can help to improve your pain and return of hip strength. Persistence in a home exercise program after physical therapy can be key to staying pain free.
Outcomes
Since a number of conditions contributes to greater trochanteric pain syndrome, outcomes can vary. For example, with conservative measures, including physical therapy and activity modifications, 25% of patients continue to have symptoms 5 years after the onset. Conservative care, including physical therapy and home exercise programs, can correct some of the underlying disease process. If symptoms do persist, injections and surgical intervention can offer patients excellent improvement in pain level, hip strength, and walking.
Greater trochanteric pain syndrome often results from one directional activities, such as running and walking; therefore, incorporating side-to-side activities and strength training can help prevent the condition from developing. If the problem develops, it is important to treat it quickly to prevent further damage, including tendon tearing. With tendon rupture and significant atrophy (loss of muscle), especially if 50% of the muscle mass is lost, the failure of surgical intervention can be as high as 75%. Under these circumstances, care includes modifying gait and using an aid, such as a walker or cane to minimize the risk of fall and fracture. Patients can develop weakness while walking, which may predispose them to falling. You should seek treatment for hip pain before significant weakness develops to decrease the risk of falling and experiencing a hip fracture, which can be life altering.
Author: Benjamin G. Thomasson, DO, FAOAO, FAAOS | Orlando, Florida
Last edited on March 7, 2025