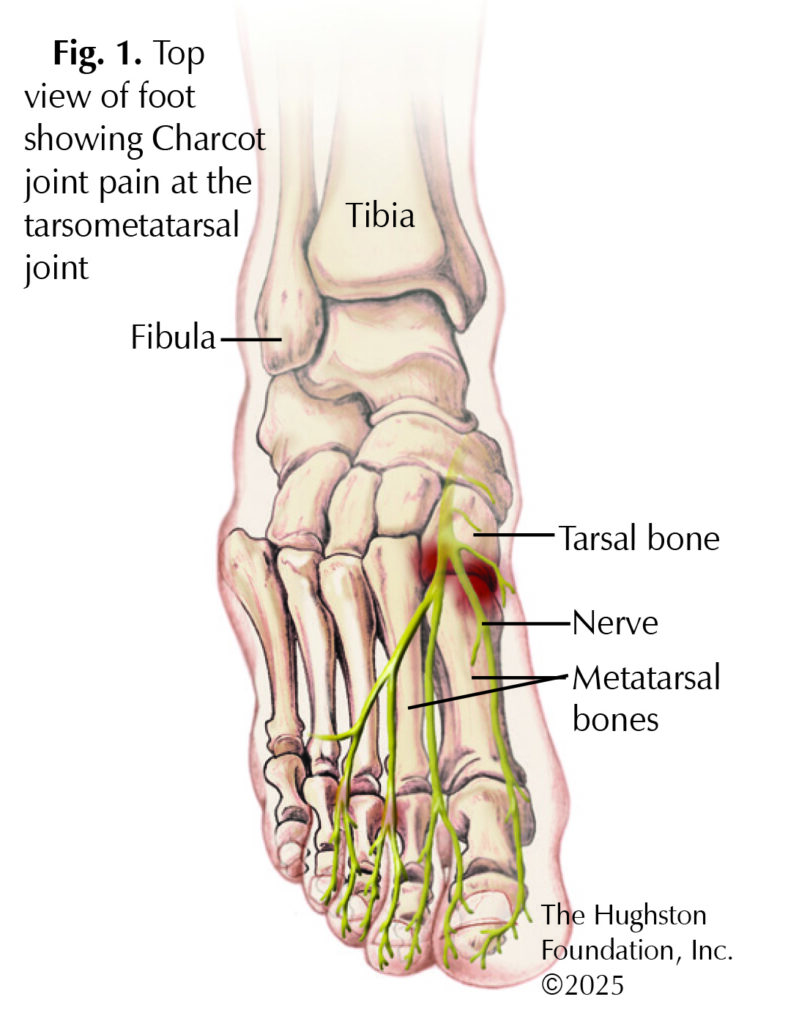
Charcot joint, or neuropathic arthropathy, is a progressive and debilitating condition characterized by the deterioration of joints due to nerve damage. Although it can occur in any condition that affects nerve function, it commonly presents in individuals with longstanding diabetes mellitus. Charcot joint typically manifests as a loss of sensation in the affected joint, leading to unnoticed trauma and repetitive stress injuries, which eventually result in joint deformity, instability, and destruction.¹ It typically affects the tarsometatarsal (connects the tarsal bone and metatarsal bone) joints (27% to 60%) (Fig. 1) and subtalar (located between the talus and calcaneus) joint (30% to 35%) of the foot, but it can present in other joints as well.²,³ The potential for severe disability and impact on quality of life emphasizes the importance of early detection, effective management, and preventive strategies. With the newly diagnosed diabetes mellitus cases exceeding 1.5 million annually in the US and an overall prevalence of 20.8 million individuals nationally, foot complications like Charcot joint are becoming more common.4

Diagnosis and symptoms
Individuals with severe sensory loss, increased mechanical joint stress, and diminished physical activity are at higher risk for development of Charcot joint. The diagnosis of the disease relies on thorough history and clinical examination. X-ray imaging is helpful in diagnosis, usually showing bone fragmentation, dislocation, or joint destruction. An orthopaedist may use magnetic resonance imaging (MRI), an image that shows the bones, muscles, tendons, and ligaments, if the diagnosis is not evident on x-ray.
The Eichenholtz classification, established in 1966, correlates imaging and symptoms to divide the disease into 3 stages: developmental, coalescent, and reconstruction.1,3,5 During the developmental stage, the ankle has swelling, warmth, and redness with bone fragmentation and joint dislocation. In the coalescent stage, the ankle warmth diminishes with a reduction in swelling and begins early stages of bone callus formation. Complete resolution of warmth and swelling with increased bone formation and bone stabilization occurs within the reconstruction phase.1 Many individuals initially experience mild to moderate pain, which progresses in later stages to painless deformity and malalignment of the joint, potentially resulting in joint collapse of the foot’s arch and dysfunctional movement..
Treatment
The management of Charcot joint aims to halt disease progression, prevent further joint destruction, and preserve function. Nonsurgical conservative approaches primarily stabilize the ankle joint and control the foot position to allow time for joint healing with intentions of preserving mobility. Initial treatment involves immobilization, nonweight-bearing and offloading the joint for 3 to 6 months, preventing further joint stress and damage. This is typically accomplished with the use of a walker boot or cast. In one study, after completion of conservative treatment and follow-up at 2 years, most patients were able to walk 6 blocks without any walking aid (walker, walking cane), with only a few patients needing an aid to walk the same distance.6
If severe instability and joint damage continues despite conservative measures, an orthopaedic surgeon may recommend surgical intervention. The surgical objectives for Charcot joint are to restore stability and alignment while preventing deformity, ultimately supporting functional ambulation. Surgical treatments include joint fusion, amputation, or total joint replacement. In the majority of cases, surgical treatment of Charcot joint results in favorable outcomes, including pain relief, functional improvement, and high patient satisfaction, with a relatively low rate of complications and revisions. The orthopaedist may recommend physical therapy during conservative treatment or after surgery to improve strength, range of motion, and function to gain as much mobility as possible.
Early recognition and management of Charcot joint are critical in preventing severe limb deformities, ulceration, and potential limb loss. Preventative measures include smoking cessation, adequate blood sugar control in diabetics, wearing appropriate socks and footwear, and avoiding walking barefoot or with open shoes. Regular diabetic foot exams to assess the extent of neuropathy and any unnoticed ulcers are among the most important preventative measures. Additionally, individuals can use custom footwear and orthotics (inserts worn in shoes) to provide support and help prevent recurrence.
Despite the challenges of Charcot joint disease, early diagnosis and timely treatment can significantly improve quality of life by preserving joint function and preventing severe disability. While the disease typically presents with symptoms like swelling, deformity, and loss of function, the absence of pain due to impaired sensation complicates early diagnosis. Effective management of Charcot joint relies on conservative measures, and in some cases, surgical intervention. Ongoing monitoring, along with a focus on preventing further joint damage, is essential for managing the disease and preventing recurrence.
Author: Aneesa A. Jones, BS | Columbus, GA
References:
- Babazadeh S, Stoney JD, Lim K, Choong PF. Arthroplasty of a Charcot knee. Orthop Rev (Pavia). 2010;2(2):e17. doi:10.4081/or.2010.e17
- Lee L, Blume PA, Sumpio B. Charcot joint disease in diabetes mellitus. Ann Vasc Surg. 2003;17(5):571-580. doi:10.1007/s10016-003-0039-5
- Trepman E, Nihal A, Pinzur MS. Current topics review: Charcot neuroarthropathy of the foot and ankle. Foot Ankle International. 2005;26(1):46-63.
- Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders. A clinical practice guideline. Journal of Foot & Ankle Surgery. 2006;45(5 Suppl):S1-S66.
- Rees H, Lyons M, Belich P, Brown N. Neuropathic (Charcot) Arthropathy of the Knee. Journal of the American Academy of Orthopaedic Surgeons. 2021;29(23):e1159-e1166.
- Gratwohl V, Jentzsch T, Schöni M, et al. Long-term follow-up of conservative treatment of Charcot feet. Archives of Orthopaedic Trauma Surgery. 2022;142(10):2553-2566.
Last edited on March 7, 2025