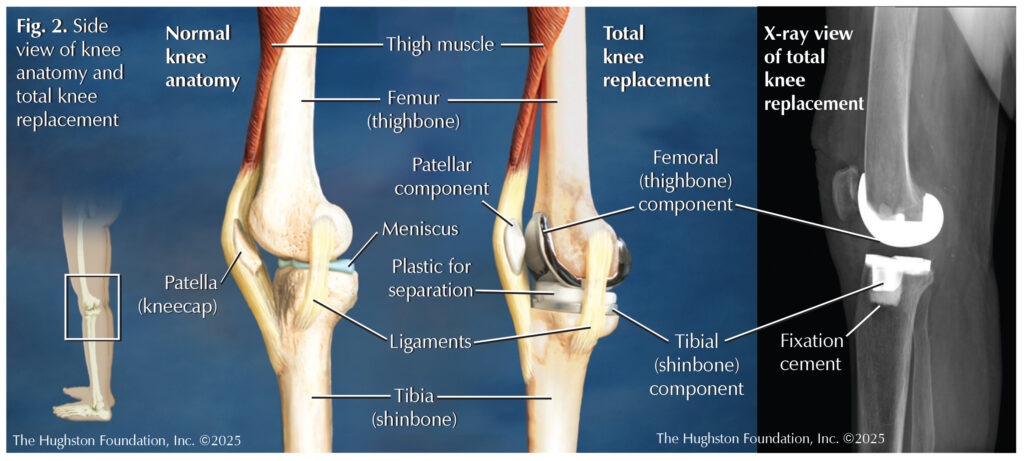
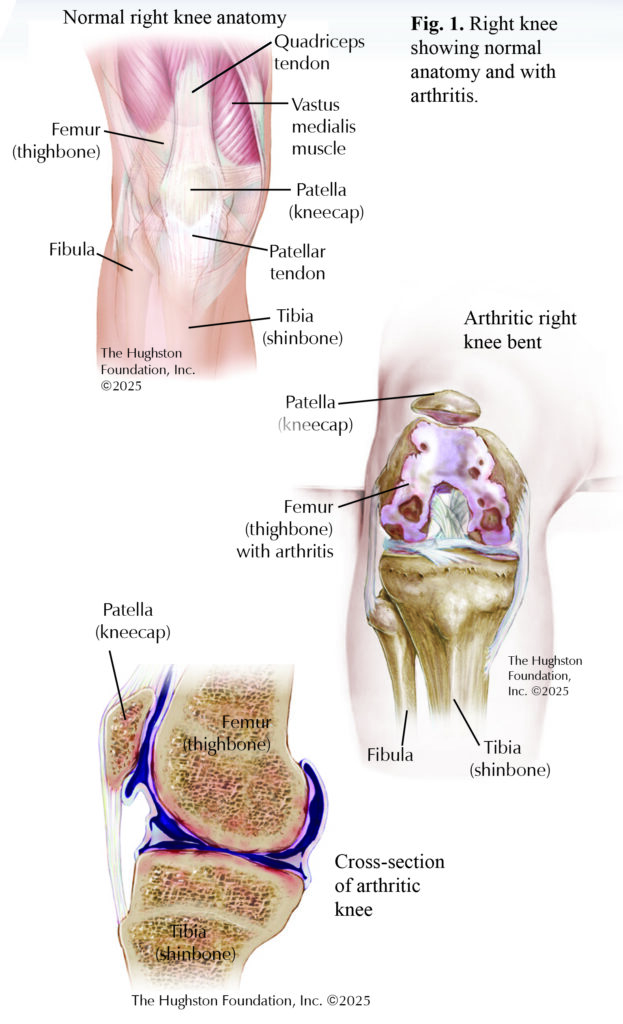
 Most knee pain is caused by osteoarthritis, a condition where the cartilage in the knee breaks down over time (Fig. 1). As the cartilage wears away, the bones in the knee can rub against each other, causing pain, stiffness, and swelling. Arthritis can also develop after a serious knee injury, such as a fracture or ligament tear, leading to long-term joint damage and pain. Rheumatoid arthritis and other autoimmune conditions cause the body’s immune system to attack the knee joint, leading to inflammation, pain, and eventual joint damage. In all these cases, knee replacement surgery can help relieve pain and
Most knee pain is caused by osteoarthritis, a condition where the cartilage in the knee breaks down over time (Fig. 1). As the cartilage wears away, the bones in the knee can rub against each other, causing pain, stiffness, and swelling. Arthritis can also develop after a serious knee injury, such as a fracture or ligament tear, leading to long-term joint damage and pain. Rheumatoid arthritis and other autoimmune conditions cause the body’s immune system to attack the knee joint, leading to inflammation, pain, and eventual joint damage. In all these cases, knee replacement surgery can help relieve pain and
restore mobility.
Knee anatomy
The knee is the largest joint in the body, connecting the femur (thighbone) to the tibia (shinbone). At the front of the joint is the patella (kneecap), which protects the knee and facilitates smooth movement. The ends of these bones are coated with smooth articular cartilage, which minimizes friction and enables the bones to slide easily against one another. Inside the knee, 2 C-shaped pieces of cartilage, known as the meniscus, act as cushions and help absorb shock. Ligaments, such as the anterior and posterior cruciate ligaments (ACL/PCL), and medial and lateral collateral ligaments (MCL/LCL) are tough bands of tissue that connect the bones and provide stability. Tendons, like the patellar tendon, attach muscles to the bone and assist in movement. Small fluid-filled sacs, called bursae, reduce friction, allowing the knee joint to move smoothly. Under normal circumstances, these components work together seamlessly, but disease or injury can disrupt this balance, causing pain, weakness, and diminished function.
Signs and symptoms
The signs of knee conditions can be similar. Common symptoms include knee pain, which may worsen with activity and stiffness that makes it hard to bend or straighten the knee. Swelling and tenderness around the knee joint are also frequent signs, and in severe cases, the knee may feel unstable or weak leading to buckling. Over time, this can lead to muscle weakness and further symptoms. People with these conditions can have difficulty walking, climbing stairs, or participating in everyday activities.
Nonoperative management
At-home treatment
For those dealing with knee pain, simple treatments at home can help manage symptoms and improve function. One of the most effective ways to reduce pain and strengthen the knee is through quadriceps strengthening exercises. The quadricep muscle, located at the front of the thigh, plays an important role in stabilizing the knee. Exercises like leg raises, squats, and straight-leg raises can strengthen these muscles, taking pressure off the knee joint and reducing pain over time. Low-impact exercises such as swimming, cycling, and walking on soft surfaces are gentle on the knees while boosting strength and mobility. These activities can improve joint mobility and muscle strength without causing additional wear and tear on the knee joint. Weight loss is also essential, as carrying extra weight puts added pressure on the knee, especially for those with osteoarthritis. Even losing a small amount of weight can make a noticeable difference in knee pain and function. Focusing on a balanced diet and engaging in regular low-impact exercise can help achieve and maintain a healthy weight.
Prescribed treatments
In addition to at-home treatments, several nonoperative treatments can be highly effective for managing knee pain. One of the most common is physical therapy. A physical therapist can create a tailored exercise plan to strengthen muscles, improve flexibility, and prevent further damage. Physicians often recommend combining nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, with physical therapy to reduce inflammation and relieve pain. Activity modifications, like avoiding high-impact activities and opting for low-impact exercises, can also reduce stress on the knee. Elevating the leg, using a knee brace, or applying ice can further assist with the swelling and discomfort.
Your doctor can recommend an injection if oral medications and activity modifications do not improve symptoms. Different types of injections exist, but the most common is a cortisone injection, which helps decrease pain through an anti-inflammatory response directly in the knee joint.
Total knee replacement
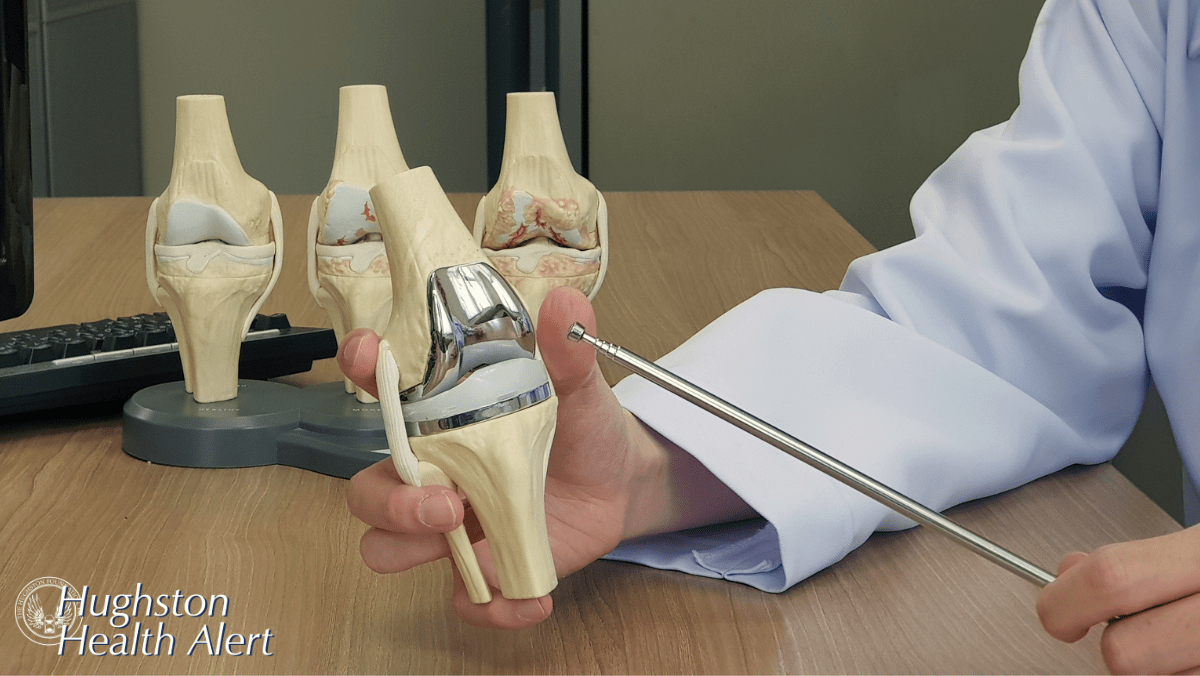
When nonsurgical treatments no longer provide relief, your physician can recommend total knee arthroplasty (TKA), or knee replacement surgery (Fig. 2). The artificial components, which are made of metal and plastic, mimic the body’s natural anatomy and movement of the knee joint. After the procedure, patients rest in a recovery area for a short time. Depending on your health, some patients are moved to a hospital room, while others go home the same day. Once you are home, physical therapy, which is an important part of the healing process, begins to help improve flexibility, strengthen the muscles around the knee, and decrease postoperative complications.
Total knee implant components
Orthopaedic surgeons use 4 basic components in a total knee replacement: 1) the femoral (thighbone) component, 2) the tibial (shinbone) component, 3) a plastic insert between the femur and tibia, and 4) the patellar (kneecap) component. During total knee arthroplasty, the surgeon cuts away the diseased ends of the femur and the tibia, and sometimes resurfaces the back of the patella. When removing the ends of the bones, the meniscus (crescent-shaped soft tissue between the tibia and femur) and the anterior cruciate ligament are removed. The medial and lateral ligaments remain in place to stabilize the replacement components. The ends of the femur and tibia are replaced with metal parts, and a plastic component replaces the meniscus between them. The surgeon can also substitute a plastic component to replace the joint surface of the patella.
Metallic orthopaedic implants are made metal alloys. An alloy is defined as a substance that has 2 or more metals fused, or dissolved, together. A cobalt-based alloy (cobalt, chromium, molybdenum) is often used in the femoral and tibial components. The cobalt-based alloy is well suited for use in joint replacement surgery because it has good resistance to wear and corrosion and it has biocompatible properties, which means the body is less likely to reject it.
Surgical approach
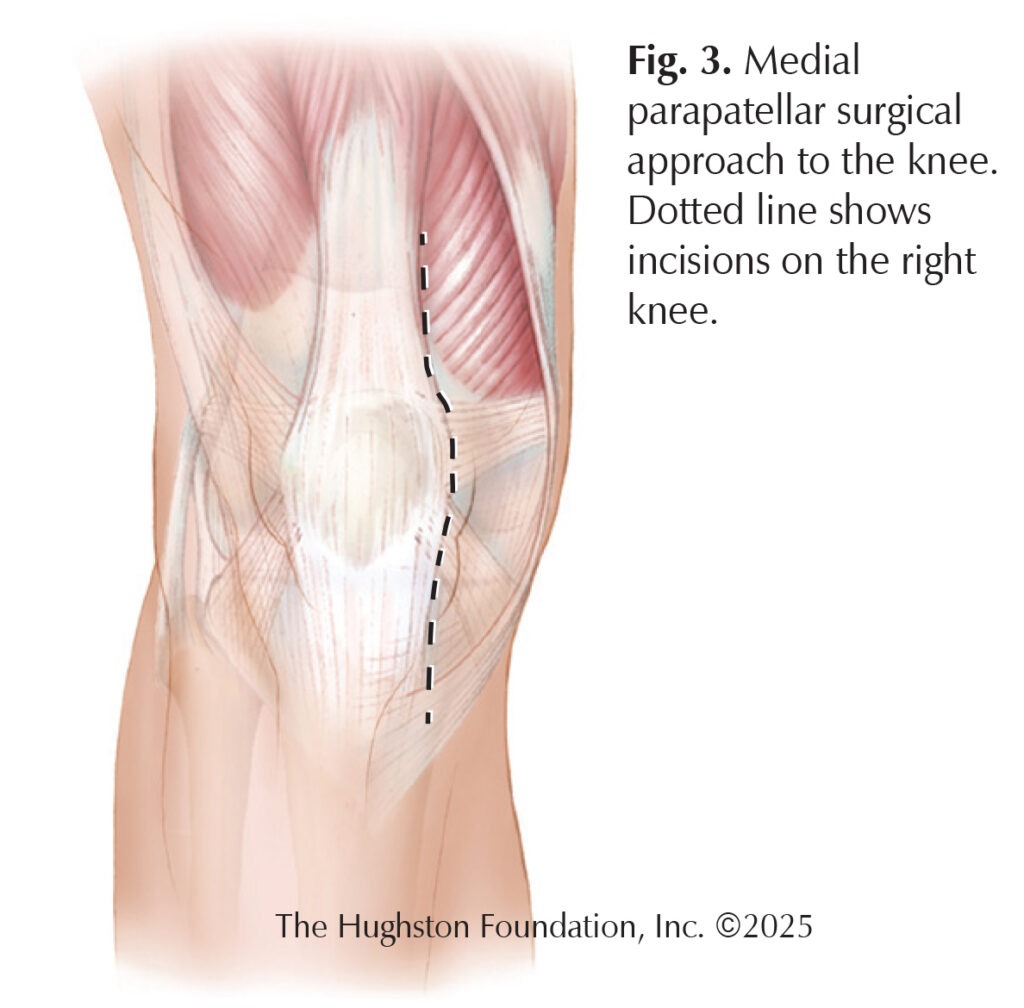
Over the years, orthopedic surgeons have refined the surgical approaches used in knee arthroplasty. The goal of the surgical approach is to gain enough exposure (allowing access and visualization of the bone) to complete the surgery while minimizing the effects to the surrounding tissues. Improvements in both technique and instruments have allowed surgeons to minimize injury to the muscles and tendons. With a trend towards shorter hospital stays, and even outpatient surgery, we continue to look for new ways to speed recovery after surgery. Each surgical approach has its advantages and disadvantages; but how the surgeon performs your surgery often depends on his or her own preference, as well as your overall health and health history.
The medial parapatellar approach has been the standard incision for orthopedic surgeons for many years (Fig. 3). The medial parapatellar incision descends down and around the patella, offering the best view of the joint. The disadvantages, however, include cutting into the quadriceps tendon, which then requires repairing. Further, the surgeon flips the patella over during the procedure, which can sometimes stretch its vascular supply.
During surgery, the metal components are securely attached, or fixated, to the bone. The surgeon can achieve fixation with a press-fit design (the textured metal creates a tight fit) or by using polymethylmethacrylate (PMMA) cement. PMMA is like a grout that holds the metal components to the bone. Moreover, the PMMA is radiopaque so the cement is visible on x-rays, and the surgeon can add antibiotics to the cement mixture to help decrease the risk of infection.
Outcomes
The outcomes of a total knee replacement surgery are generally very positive, especially for people who suffer from chronic knee pain due to conditions like arthritis or injury. While the recovery process can take time, many people experience significant pain reduction and improvement in their ability to walk, run, or jump. Most people are back to full activities about 3 months after the operation, but full recovery can take up to a year.
In the long term, total knee replacements can last 25+ years, although it depends on the individual and activity level. Overall, many people are very satisfied with their total knee replacement. It allows them to return to normal activities and enjoy a better quality of life, free from the constant knee pain they experienced before the surgery.
When is the right time?
In most cases, joint replacement surgery is elective, meaning the timing is up to you. The decision largely depends on the level of pain and impact on function. If you’re experiencing severe pain in your knee that makes it difficult to move, walk, or climb stairs, it’s time to consult with your doctor. If nonoperative treatments do not provide relief, surgery can be a reliable and effective solution to help you return to an active lifestyle with reduced pain.
Authors: Andrew Bae, DO, and Gina Bae, BS, OMS-IV | Nashville, Tennessee
Last edited on July 15, 2025