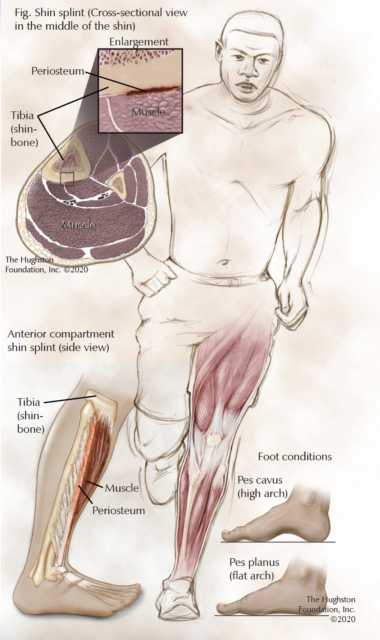
 Shin splints, known as medial tibial stress syndrome, are a common sports injury incidental to overuse activities (Fig.). Orthopaedists and athletic trainers frequently see medial tibial stress syndrome in military recruits and athletes, specifically when their activity or sport requires repetitive running and jumping. While often not a serious health issue, shin splints can be disabling and, without proper management, can progress to more serious conditions. Fortunately, with early recognition and proper management, shin splints are a very manageable condition.
Shin splints, known as medial tibial stress syndrome, are a common sports injury incidental to overuse activities (Fig.). Orthopaedists and athletic trainers frequently see medial tibial stress syndrome in military recruits and athletes, specifically when their activity or sport requires repetitive running and jumping. While often not a serious health issue, shin splints can be disabling and, without proper management, can progress to more serious conditions. Fortunately, with early recognition and proper management, shin splints are a very manageable condition.
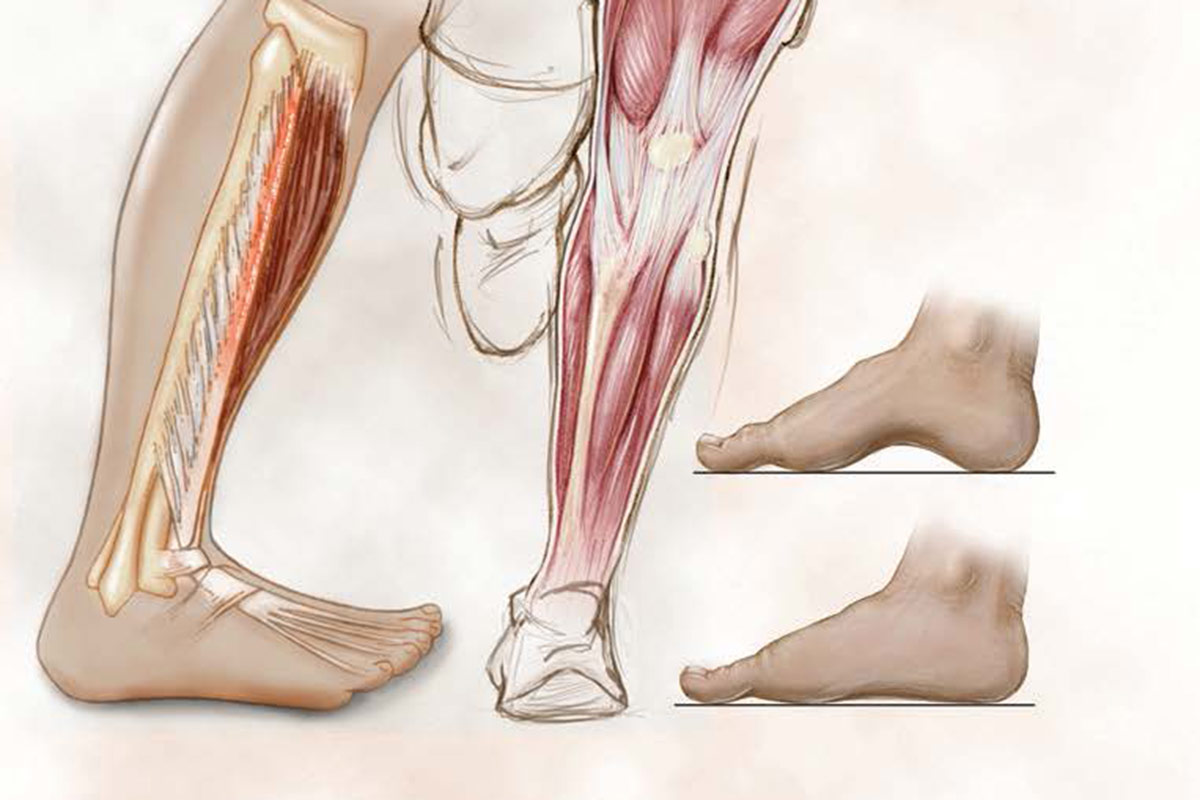
Shin splints are an overuse, repetitivestress injury that results in periostitis (inflammation of the tissue surrounding a bone) at the posterior medial (inner) border of the distal tibia (shinbone). Historically, clinicians considered the tibialis posterior muscle the primary source of shin splints, but studies have also identified other lower leg muscles including the soleus, tibialis anterior, and flexor digitorum longus as possible sources of the condition. The cause is often multifactorial and involves both abnormal biomechanics and training errors.
What are the symptoms?
People suffering from shin splints typically notice pain, specifically in the lower two-thirds of their tibia, which can be painful to touch. The pain is usually a vague, dull, achy pain that becomes intense with activity, is noticeably worse at the beginning of exercise, and gradually subsides during activity or shortly after cessation of exercise. However, as the injury progresses, pain may be present with everyday activity and even at rest.
Diagnosing shin splints
An orthopaedist can often diagnose shin splints after taking a thorough patient health history and performing a physical examination. Additionally, your doctor may inquire about your type of activities, the duration of the activity, and the type of footwear you use. The physical examination can include assessment of your flexibility, particularly in the lower extremity, strength, neurovascular status (sensory and motor function), and any lower leg or foot abnormalities. These abnormalities can include knee alignment, leg length differences, rotational difference, and pes cavus (high arch) or pes planus (flat arch) of the feet. Examination of the core muscles, spine, and pelvis may also reveal imbalances that can contribute to dysfunction in the lower extremity.
Your orthopaedist may order imaging studies if he or she is suspicious that stress fractures are causing your pain. Because shin splints can progress without proper treatment, your doctor may opt to order radiographs (x-rays), bone scans, or magnetic resonance imaging (MRI scan that shows bones, muscles, tendons, and ligaments) in order to rule out fractures or other injuries and diseases.
How do you treat shin splints?
Your initial treatment for shin splints primarily focuses on pain and inflammation reduction. Your doctor may instruct you to reduce activity and take a break from your sport or training activities for 2 to 6 weeks. During that time, you should apply ice 3 to 4 times daily for 15 to 20 minutes and take nonsteroidal anti-inflammatory medications (NSAIDS), such as naproxen sodium or ibuprofen, to control pain and reduce inflammation in the affected area. Additionally, you may benefit from physical therapy modalities including ultrasound, whirlpool, phonophoresis (uses ultrasound and topical medications), soft tissue management, and electrical stimulation which can help reduce pain and promote tissue healing. In severe cases, you may need to remain nonweightbearing for a period of time, which means you may need to use crutches and wear a cast to relieve the stress placed on the lower extremity.
After initial treatment, your orthopaedist will focus on long-term management and prevention of recurrence, by modifying your training program and addressing any biomechanical abnormalities. Decreasing activity frequency, intensity, and duration by 50% often improves symptoms without completely stopping activity. Additionally, you are encouraged to avoid running on uneven, firm surfaces as well as up or down hills since these activities increase the stress placed on the lower leg musculature. Transitioning to a synthetic track or comparable surface is a good way to continue activity while not causing further injury. You can also replace or change your training with low impact exercises such as water aerobics, swimming, stationary biking, or using an elliptical machine.
To address biomechanical problems, your physician can recommend that you use proper footwear or orthotics for your sport or everyday activities. Shoes, specifically those used during training activities, should have sufficient shock absorption in order to reduce the forces transmitted into the lower leg. Shoes should fit properly and you may need to alternate with another pair if they are wet, since this can compromise the support. You should replace your shoes between 250 and 500 miles as distances beyond this tend to decrease their shock absorption and support by up to 40%. If you have flatfeet or foot malalignment, over-the-counter or custom orthotics can be beneficial.
During all phases of treatment, you should place emphasis on improving lower extremity flexibility and strength. Calf stretching, lower leg strengthening, and core stability exercises can be demonstrated to you and performed at home multiple times a week in order to prevent recurrence.
Manual therapies to improve or correct musculoskeletal abnormalities may be used. Your therapy should focus on areas with imbalance that affects the lower extremity, such as the spine, sacroiliac joints, and pelvis. Your orthopaedist and physical therapist can use osteopathic manipulation and physical therapy to address these dysfunctions. You can incorporate proprioceptive training with a 1-legged stance, wobble, or balance board into the manual therapies to increase postural stability and improve the musculoskeletal support required during training activities.
In cases that do not respond to nonsurgical treatment, injections with substances that promote local healing such as platelet-rich plasma or surgery that focuses on the problematic musculature are often successful. If your treatment fails to bring you relief, your orthopaedist will discuss more invasive options to alleviate your pain.
How can you prevent shin splints?
If you have a history of shin splints or if you are beginning a new workout routine, you should pay particular attention to the prevention of shin splints. You should focus on your flexibility, proper footwear, core and lower extremity strengthening, as well as training in moderation especially when beginning a new program. Physicians, physical therapists, and athletic trainers can help educate you as well as demonstrate the proper techniques to use for prevention.
Author: Benjamin J. Catoe, DO, ATC | Columbus, Georgia
Last edited on October 18, 2021