Contributing physicians in this story
We are seeing a steady increase in the prevalence of knee arthritis affecting adults in the United States. In fact, more than 10% of men and women over the age of 60 have symptomatic arthritis, which likely arises from an increase in the population’s age and adults who are more active. Unfortunately, the pain and instability of knee arthritis can greatly affect your quality of life and overall mobility.
When the symptoms first begin, patients often use braces and over-the-counter pain relieving creams and medications; however, as arthritis advances, symptoms can become unresponsive. Your physician may recommend physical therapy or intra-articular (inside the joint) steroid injections. If these nonoperative treatments fail, your doctor may recommend total knee replacement. Researchers project that by the year
2030 surgeons will perform approximately 1.2 million total knee arthroplasty (replacement) (TKA) procedures each year.
 What types of arthritis affect the knee?
What types of arthritis affect the knee?
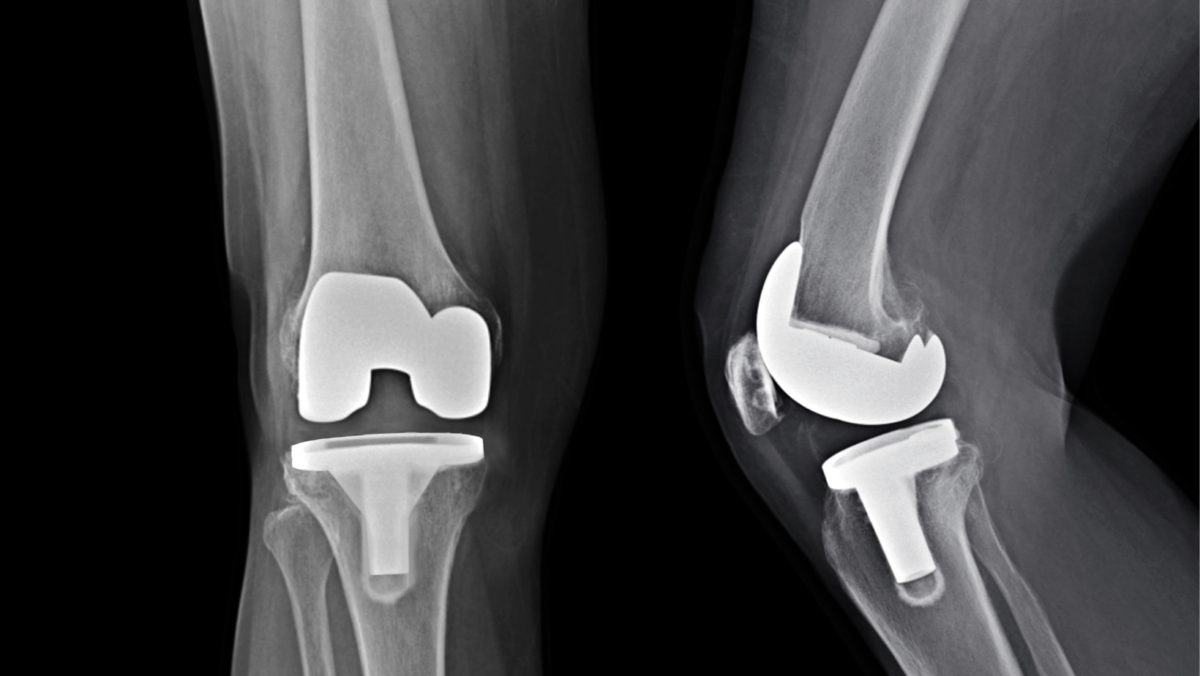
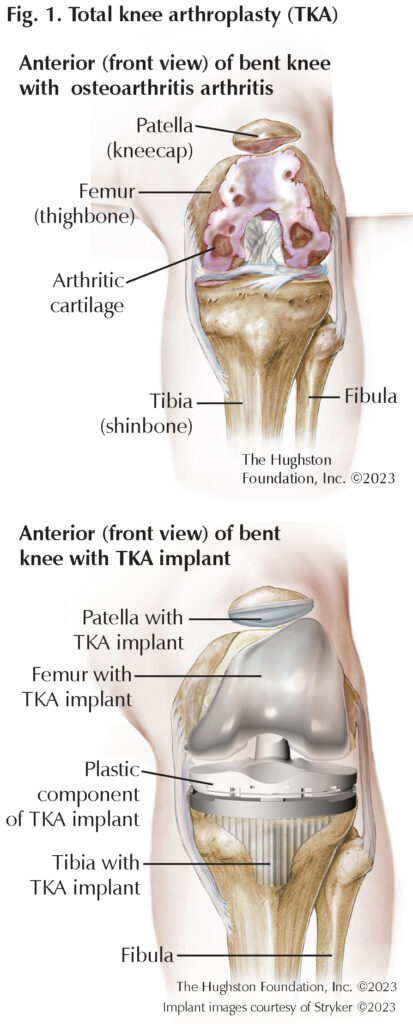
There are 3 major types of arthritis that doctors see in the knee: primary osteoarthritis (OA) (Fig. 1), post-traumatic osteoarthritis, and inflammatory arthritis. Primary osteoarthritis is the most common type of arthritis orthopaedic surgeons treat because it results from normal wear and tear on joints and may have a genetic component. Post-traumatic osteoarthritis, which results from an injury to the knee that occurred years prior, can be from sports, trauma, or infection that damaged the surrounding ligaments (tissue that connects bones) or cartilage (hard slippery tissues that cover the ends of bones) that over time has led to deterioration of the joint. Another common type of arthritis, inflammatory arthritis, is seen in patients who have autoimmune disorders (the body’s immune system attacks healthy tissue, including joints), such as rheumatoid arthritis or psoriatic arthritis. A rheumatologist often manages these types of arthritis with medications. Despite the treatment, unfortunately the result is often joint destruction and an eventual need for knee replacement.
Why does my knee hurt?
There are several reasons why knee arthritis can cause pain. In the early stages, the cartilage of the joint begins to degenerate, leading to inflammation within the joint, which produces enzymes that trigger pain receptors. As the cartilage continues to wear, the space within the joint reduces allowing the bones to move closer together. As the joint space narrows, the supporting ligaments loosen and the knee becomes unstable. With activity, this instability causes the ligaments to stretch and activates the pain fibers around the knee. In the last stages of arthritis, the cartilage can completely wear away producing bone-on-bone contact. The mechanical grinding of bone against bone causes significant pain and loss of function.
What are the nonoperative treatments for knee arthritis?
Although treatment recommendations depend on the severity of your symptoms, all patients warrant an attempt at nonoperative care. You should take simple measures first, including changes in activities and maintaining a healthy weight. For active patients, changing workout routines that lessen the impact on your knees may be beneficial, such as substituting higher impact exercises with low-impact aerobics. Physical therapy for lower leg muscle strengthening can help with mild to moderate knee arthritis as increasing muscle strength can compensate for the deteriorating knee joint and associated instability. At the same time, over-the-counter and prescription anti-inflammatory medications including ibuprofen, naproxen sodium, diclofenac, meloxicam, and celecoxib can relieve some of the discomfort. Acetaminophen is also an effective pain reliever with fewer gastrointestinal side effects than anti-inflammatories.
Additionally, knee braces can help with mild to moderate arthritis and they range from inexpensive compression sleeves to medical-grade hinged devices. Knee braces provide added stability for deteriorating knee cartilage, as well as increase sensory feedback, known as proprioception, on the knee’s position in space. This feedback helps with knee stability, which subsequently reduces pain.
Furthermore, intra-articular injections are a successful nonoperative treatment option performed by orthopaedic physicians. Most injections consist of a combination of local anesthetics and corticosteroid. These types of injections reduce inflammation within the joint leading to pain reduction. Viscosupplementation (a gel-like fluid, consisting of hyaluronic acid) is another injection option that may provide significant relief. These injections add lubrication to the joint for decreased pain with movement and some studies have indicated they may also have the added benefit of anti-inflammatory properties.
Who is a candidate for a total knee replacement?
Surgeons consider total knee arthroplasty for patients who have end-stage arthritis of the joint. Usually, patients who have had at least 6 months or more of symptoms and have failed to have significant relief with nonoperative treatments including medications, injections, physical therapy, and activity modifications are candidates for knee replacement. The patient’s radiographs (x-rays) usually show bone-on-bone contact between the femur (thighbone) and tibia (shinbone). Some patients, especially those with inflammatory arthritis, may not progress to end-stage arthritis before the pain becomes severe enough for knee replacement.
Total knee replacement is a major surgery; therefore, the patient must be healthy enough to undergo the surgery and complete postoperative rehabilitation. To prepare for knee replacement, your primary care provider will complete a physical to ensure that you are healthy enough for surgery and will usually order a chest x-ray, electrocardiogram (EKG) of your heart, and basic blood work. Patients who have medical conditions may need clearance from specialists, such as a pulmonologist (respiratory specialist) or cardiologist (heart doctor).
How is a total knee arthroplasty performed?
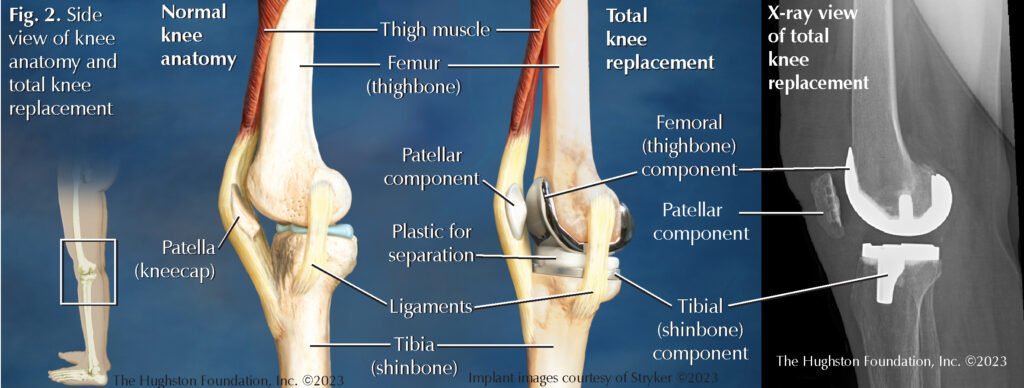
Total knee replacement is performed through an incision about 6 to 8 inches in length in the front of the knee. The surgeon can perform the surgery using general anesthesia or spinal anesthesia and a local nerve block (injection) for postoperative pain control. Surgery typically lasts about an hour and involves removing part of the end of the thighbone and top of the shinbone. The surgeon then covers the surfaces with properly sized metal implants and inserts a piece of medical grade plastic in between (Fig. 2). The surgeon closes the incision in layers and covers the wound with a sterile dressing. Patients who are otherwise healthy and are able to ambulate can go home the same day, but some people may require a 1- to 2-night stay in the hospital for proper pain control and physical therapy.
Is there a preferred technique or method?
Although numerous companies make knee replacement implants, studies do not show that any particular device is superior to any other. Most orthopaedic surgeons use a few implant companies that they are familiar and comfortable with. Surgeons often secure the implants to the bone with a specialized bone cement. This is a grout-like material that the doctor mixes in the operating room and places on the bone along with the implant. The surgeon then holds the new parts in place while the cement hardens. A newer technique for implants does not involve cement. These types of implants have a specialized coating on the underside that contacts the bone. This coating allows the bone to grow onto the implant providing a secure fit to the bone end. No current studies show that any type of implant fixation is superior to the other. Other exciting technologies deal with how the surgeon cuts the bone during surgery. Your surgeon may discuss methods, such as computer assisted navigation, custom cutting guides, as well as robotic assisted surgery. These are all new technologies that may offer advantages over conventional surgery; however, the approach or method is often your surgeon’s preference and what is best for you.
What happens after surgery?
Physical therapy is the most important part of recovery and begins on the day of surgery. Therapy starts with walking and bending the knee to maintain range of motion. Patients must begin moving the knee right away to prevent stiffness. The therapist can help with maintaining motion and instructing patients on exercises. This motion will be uncomfortable at first but tends to get better over the first few weeks of recovery. You will have multiple therapy visits each week and patients are to perform exercises at home as well. Although patients may need a walking aid such as a rolling walker or cane, within the first few weeks, most patients can ambulate without assistance by their 6 weeks follow-up appointment.
What are some potential complications?
The most dreaded complication following knee replacement is infection. For this reason, your surgeon will prescribe a dose of antibiotics before the procedure and usually at least 1 or 2 doses after surgery to reduce your risk of infection. Should an infection arise, treatment ranges from oral antibiotics if it is localized to the skin, or you may need further surgery for cleaning the joint if the infection appears to be around the implant components.
Additionally, blood clots can form in the leg after a knee replacement because of the surgery and decreased activity. For that reason, your doctor may place you on a blood thinner for up to 6 weeks after surgery. If you have few risk factors and are relatively healthy, you may only need aspirin. If you have a few medical problems or a history of previous blood clots, your doctor may prescribe a stronger blood thinner medication or an injection.
Stiffness is also a feared complication. This is why physical therapists stress early and frequent motion during rehabilitation. If stiffness persists and limits function, a return to the operating room for a manipulation may be necessary to regain motion. After the manipulation, the patient will restart an aggressive physical therapy regimen. The best way to prevent complications is to follow the postoperative instructions provided by your orthopaedic surgeon.
What are the outcomes of knee replacement?
The vast majority of patients have significant improvements in pain and function following total knee arthroplasty. Recovery can vary but most patients have improvement with decreased pain at 6 weeks after surgery. With proper therapy and activity, improvements in pains and function will continue for 6 months to 1 year after surgery. You may experience occasional aches and pain around the knee implant with weather changes and increased activity. The hope is that only over-the-counter pain medications are necessary to control these minor aches and pains. Active patients can often return to recreational activities without restriction; however, you must take care to avoid excessive strain on the joint, which can affect its longevity.
Author: Benjamin J. Catoe, DO, and Randall J. Ruark, MD | Columbus, Georgia
Last edited on November 15, 2023