Contributing physicians in this story
The bones and bone marrow of the human body are living tissues with cells that require an adequate blood supply to remain healthy. If blood flow to these bone cells decreases or stops, the supply of essential nutrients and oxygen ultimately leads to cell death. This can lead to localized bone collapse if it occurs within the marrow. Orthopaedists refer to this cycle of decreased blood flow and cell death as osteonecrosis, but physicians also refer to it as aseptic necrosis or ischemic necrosis of bone. Osteonecrosis can occur as a localized process of a single joint or as a systemic (affects the whole body) event. Osteonecrosis can happen to any bone, but the elbows, ankles, feet, wrists, and hands are less commonly affected. Often, it develops at the ends of the long bones of the femur (thighbone) and humerus (upper arm bone). When cell death and bony destruction occur adjacent to a joint surface, it can lead to the collapse of the joint surface and progressive destruction of the joint space.
What causes osteonecrosis?
Trauma or repetitive microtrauma to the bone adjacent to a weight-bearing joint can cause localized osteonecrosis. Systemic or multifocal (3 or more sites) osteonecrosis can also occur. Many factors are capable of triggering osteonecrosis, such as exposure to high-dose glucocorticoids (steroid medication), sickle cells (red blood cell disorder), nitrogen bubbles (caisson disease), excessive alcohol consumption, or blood clotting abnormalities. Connective tissue disorders, such as systemic lupus erythematosus, and metabolic disorders, such as hyperlipidemia, have been associated with the development of osteonecrosis. Cytotoxicity (chemotherapy) and genetic factors could also be involved. Cellular injury may ensue regardless of the precipitating mechanism, leading to critical ischemia (restricted blood flow) and cell death. However, osteonecrosis remains uncommon even if the patient is exposed to one of these numerous risk factors.
Osteonecrosis of the foot and ankle
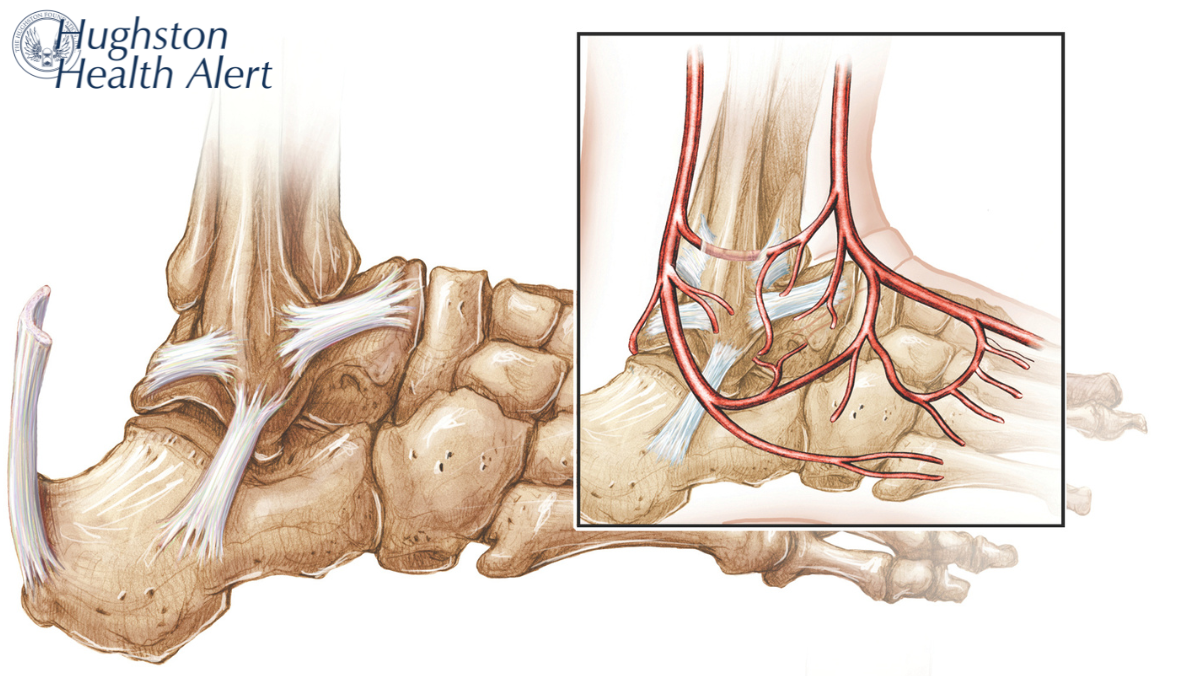
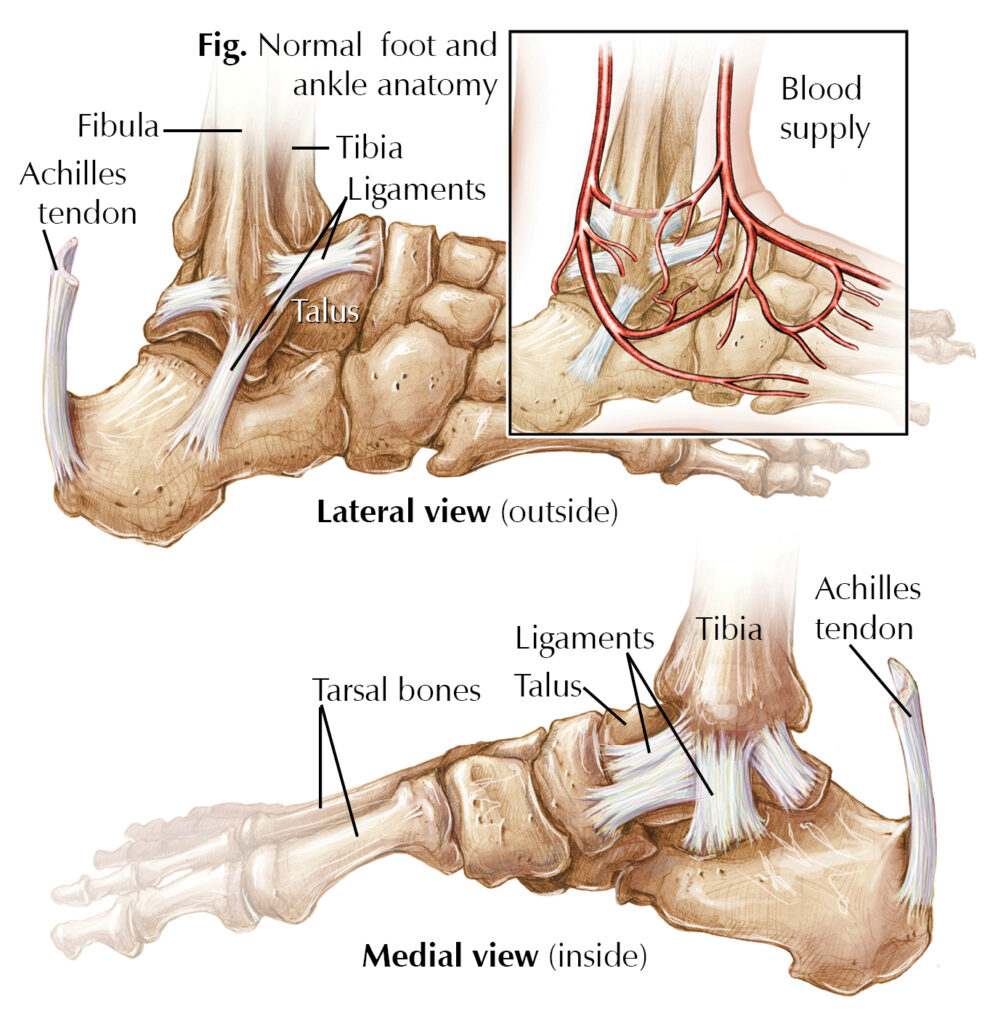
Remarkably, 25% of the bones in the body are found in our feet (Fig.). The foot and ankle form a complex structure consisting of 28 bones and 33 joints. The skeletal structure of the ankle, or tarsus, has 7 bones. The talus bone articulates above with the bones of the lower leg (tibia and fibula) to form the ankle joint. The other 6 tarsal bones are tightly bound together by ligaments (tissues connecting bone) below the talus and function as a strong weight-bearing platform. Osteonecrosis of the talus can result from many conditions; however, trauma is the most common cause of damage to the fragile blood supply of the talus. Idiopathic (an unknown cause) and spontaneous osteonecrosis of the isolated tarsal bones in the foot and ankle can occur. In approximately 10% of the osteonecrosis cases, the cause remains unknown.
Nonsurgical treatment
Physicians can treat osteonecrosis nonoperatively, focusing on preventing further damage to articular cartilage (covering the ends of bones). Nonoperative management can be successful in cases with early diagnosis, and its primary aim is to protect the bones involved until revascularization (procedure to restore blood flow) can occur. Treatment regimens consist of periods of nonweight bearing or partial weight bearing using splints and braces as needed. These methods reduce the breakdown of bone and decrease the progression of articular joint damage.
Surgical treatment
Surgical treatment options can be divided into 2 categories: joint-sparing or joint-sacrificing. Joint-sparing techniques are used in the early stages of osteonecrosis, including core decompression and vascularized bone grafting. During core decompression surgery, the surgeon drills the avascular bony region and removes the diseased bone, allowing blood flow to reach the area. Vascularized (contains blood vessels) bone grafting similarly allows for a new, vascularized segment of bone to be inserted. In joint-sacrificing procedures, the surgeon replaces the existing necrotic bone with an implant or a fusion across the affected joint space. The surgeon may perform a talar replacement with a custom metal implant, depending on the patient.
Authors: Harley L. Ponder and Collier B. Watson, DO | Columbus, Georgia
Last edited on September 13, 2024