Contributing physicians in this story

For many reasons 2020 was a challenging year. In particular, it made practicing medicine challenging because many patients had been worried about visiting their doctors for fear of exposing themselves to COVID-19. This left patients searching for answers online. Although the Internet has a wealth of information available, a quick search of symptoms for hand pain and stiffness can be overwhelming. As an orthopaedic hand surgeon, one of the most common presenting complaints is hand pain related to arthritis. Fortunately, when I see these patients, I am able to offer both nonsurgical and operative solutions. When it comes to musculoskeletal disorders of the hand, the key is receiving the appropriate examination, diagnosis, and treatment from an orthopaedic physician who specializes in treatment of hand injuries and disease.
Changes in the hand
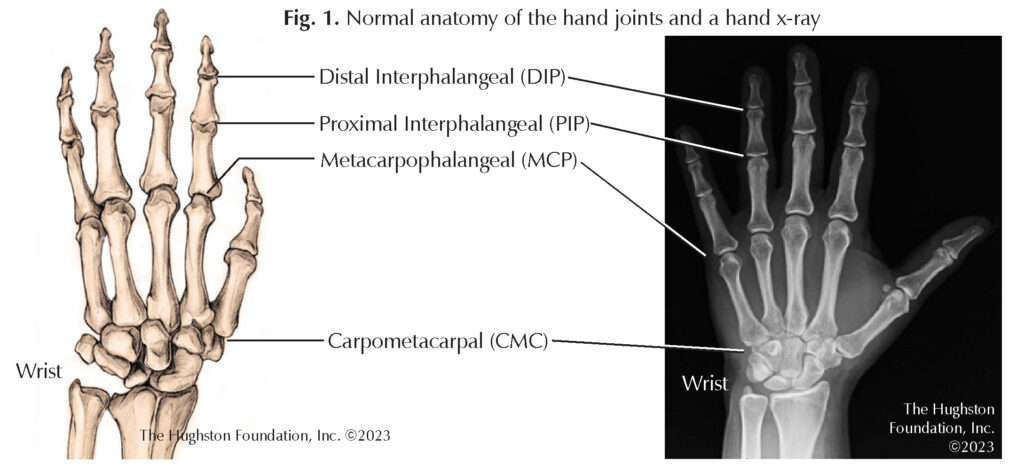
Hand arthritis is a common term used to describe the degenerative changes that take place within the small joints of the hand. Arthritis can have varying causes including: osteoarthritis (a degenerative disease caused by overuse), post-traumatic injury, or inflammatory, which is related to metabolic or autoimmune disorders, such as gout, pseudogout, rheumatoid, or psoriatic arthritis. The hand comprises all structures beyond the wrist joint and contains many different bones, tendons (tissues connecting muscle to bone), nerves, and vascular structures. The joints of the hand include the carpometacarpal (CMC), the metacarpophalangeal (MCP), the proximal interphalangeal (PIP), and the distal interphalangeal (DIP) bones (Fig. 1).
Osteoarthritis refers to the constellation of radiographic (x-ray) findings associated with wear and tear of the joint cartilage that has no other underlying cause. When cartilage breaks down, the joint loses its natural shock absorber; and therefore, the force transmits to the bone. X-rays may show a narrow joint space that depicts bone-on-bone disease. Additionally, bone spurs or cysts are common findings in patients presenting with osteoarthritis. Additionally, patients often experience inflammation, pain, and swelling around the joint.
Those at risk for developing osteoarthritis are typically elderly patients with a history of overuse of the hands. Furthermore, recent studies have linked osteoporosis to degenerative changes throughout the body including thumb basal joint arthritis. Therefore, primary care physicians should screen patients who are at risk for osteopenia or osteoporosis and discuss medical management for these diseases. Physicians may recommend patients to take vitamin D, calcium, or other anti-bone resorption supplements.
Nonsurgical treatment
Physicians approach the treatment for arthritis in the small joints of the hand differently than the larger joints in the body. Patients may present with “start up” pain related to the initiation of motion. Hand surgeons encourage finger range of motion exercises to minimize the risk of stiffness. The mainstay of treatment for hand arthritis relies on maximizing nonoperative modalities such as ice, heat, and anti-inflammatory medication. For stiffness, heat can help to loosen the connective tissue in the muscles, tendons, and ligaments (tissues connecting 2 bones) and may improve overall range of motion. Ice can help to minimize swelling, inflammation, and pain. Anti-inflammatory medications such as ibuprofen, naproxen, and meloxicam can help patients overcome a particular flare-up and minimize the inflammatory cascade that results in pain.
Unfortunately, there are patients who present with unrelenting symptoms despite nonsurgical treatment. Depending on the diagnosis, intermittent steroid injections may help to ease symptoms. Basal joint arthritis is the most common location for primary arthritis in the hand and often responds well to a steroid injection. According to a 2015 article in the Hand journal, when comparing placebo, hyaluronic acid, and steroid injections for thumb arthritis, only steroid injections demonstrated any long-term clinical improvement in symptoms. However, physicians should inform patients that symptoms could return after an injection because the steroid medication does not change the underlying degenerative injury to the joint.
Surgical treatment
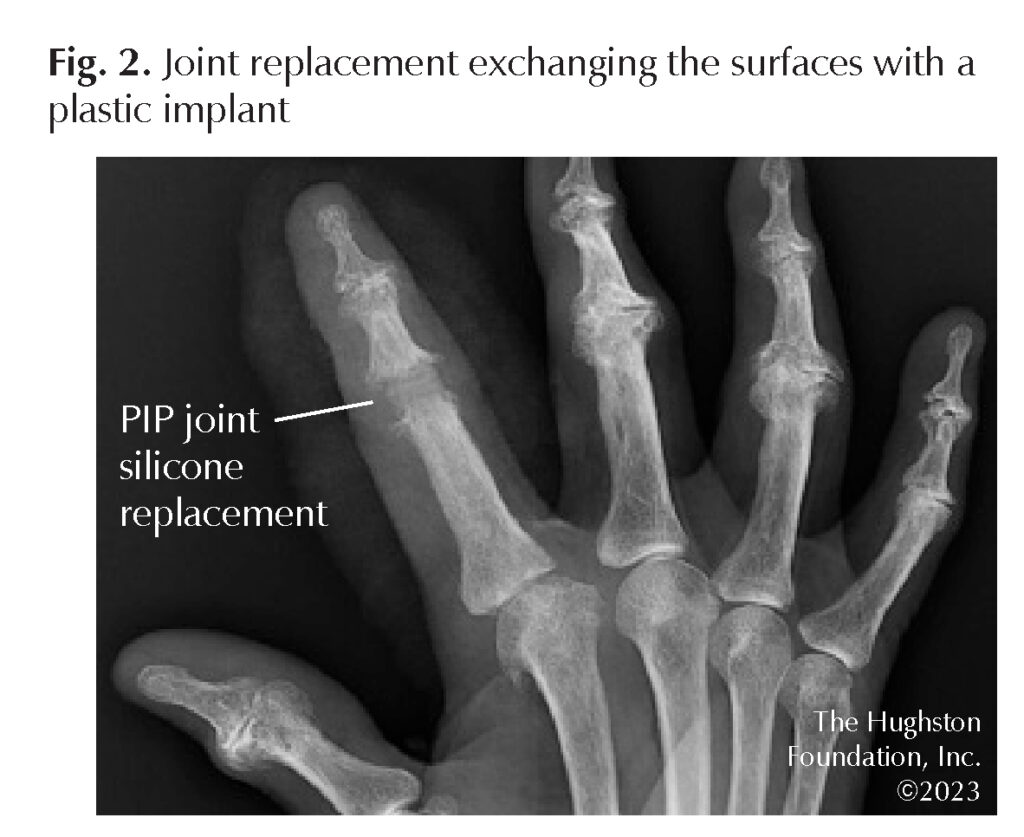
Surgical treatment varies based on the joint in question, though the options are to either replace the joint or fuse the joint. A joint replacement procedure eliminates the arthritic joint by exchanging the surfaces with metal and plastic implants (Fig. 2). A fusion procedure eliminates the arthritis by permanently connecting 2 bones together (Fig. 3). Joint replacement affords the ability to maintain motion whereas fusion inhibits motion. However, both procedures help to eliminate pain.
Additionally, each procedure has its own rehabilitation regimen. Joint replacement allows for early range of motion to minimize the risk of joint stiffness. On the other hand, patients undergoing a joint fusion require a longer period of disuse, typically until the fusion takes. This could be several weeks to months depending on the patient’s risk factors, such as other medical problems, or a history of smoking. Patients must also minimize the stress at the joint level following a joint fusion because too much stress can result in broken hardware or a nonunion.

As one can imagine, the outcomes vary depending on the patient’s demand and the type of procedure performed. However, patients are generally pleased with surgical treatment because the goal is to minimize pain. Postoperatively, most patients will engage in a treatment protocol involving home exercises and physical therapy. Therapists can help with scar desensitization, motion, and strength training. Working on strength training of the small muscles of the hand is just as important as exercising the larger muscle groups in the body. Small joint exercises may be tedious but formal therapy can result in better overall outcomes and improved patient satisfaction.
Risk factors
Repetitive movements, advanced age, family history, and hand trauma are just a few risk factors for hand arthritis. Osteoporosis can lead to degenerative changes in the body, including the hands; therefore, to maintain good bone health patients should have appropriate vitamin D and calcium levels. Researchers also believe that smoking cessation leads to better pain control and improved efficacy of corticosteroid injections. In terms of post-traumatic arthritis, the only way to minimize the risks are to minimize the dangerous activities that can result in such trauma but more so, to seek early medical attention. Following an injury, a patient should have an x-ray to determine the extent of injury or whether specialty care is needed. Fractures that are missed and diagnosed weeks or months later can result in significant disability.
See a hand specialist
Arthritis is only one of many reasons you may be experiencing hand pain. Managing symptoms may help to avoid invasive procedures and eliminate the need for surgical treatment. If you do find yourself requiring treatment, research your local or regional fellowship-trained hand surgeon for the best care.
Author: Todd Rubin, MD | Nashville, TN
Last edited on December 5, 2023