Contributing physicians in this story
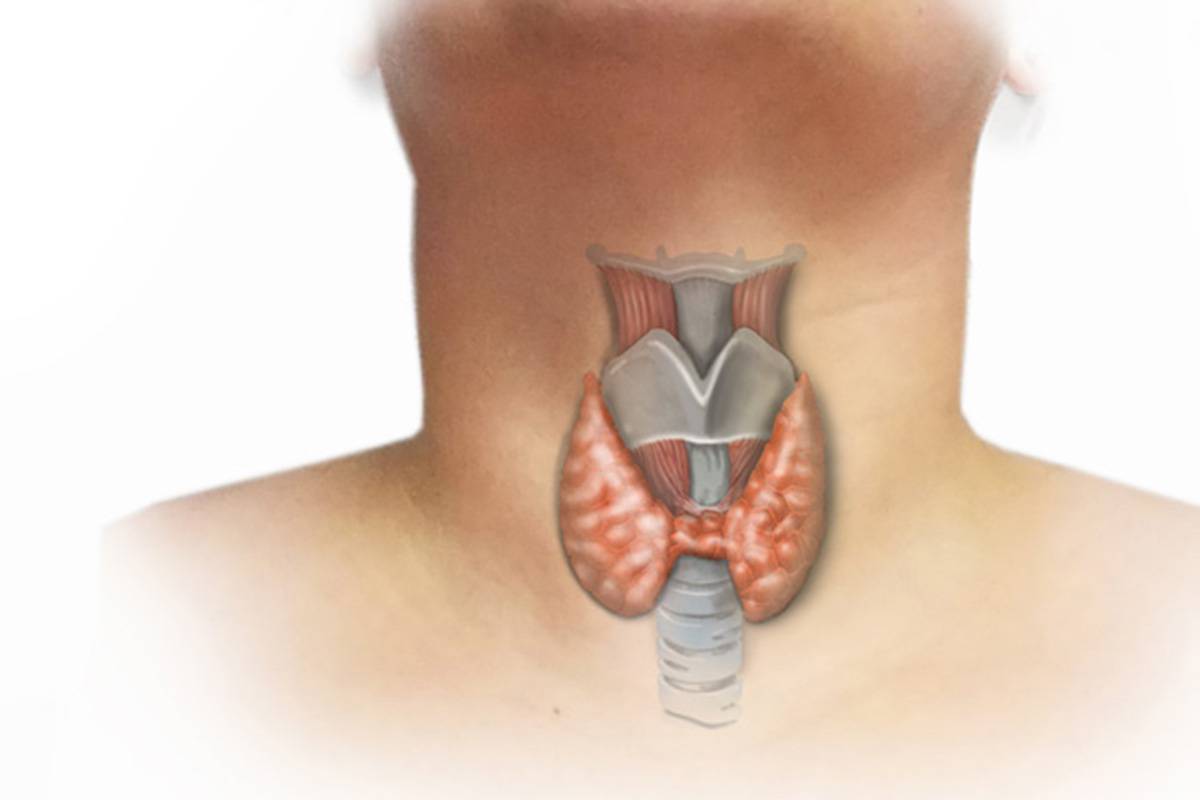
Thyroid disease comes in many forms, but not all thyroid disease requires surgical attention. If you detect an abnormal lump or swelling in your neck or if you begin to experience symptoms suggestive of an overactive thyroid gland, contact your primary care physician (Fig). These symptoms can include intolerance to heat, unexplained weight loss, muscle weakness, tremors, fatigue, skin and hair quality changes, new onset of nervousness, anxiety, or heart palpitations. 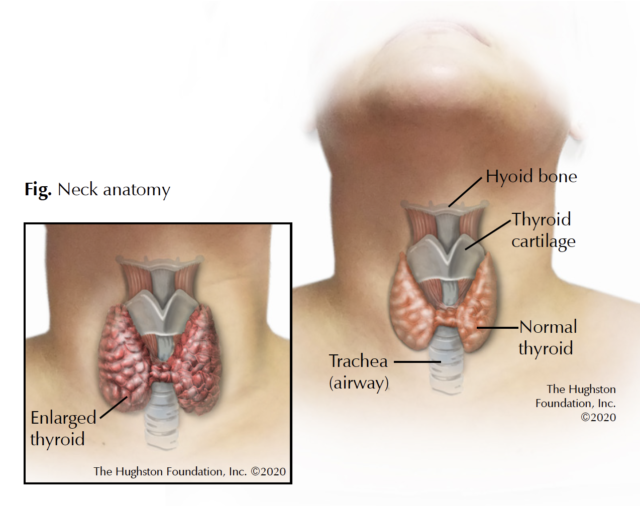
There are diseases of thyroid function, which we often describe as either hyperthyroidism (an overactive thyroid gland) or hypothyroidism (an underactive thyroid gland). Then there are diseases that affect the thyroid’s physical form, which we often describe as either a goiter (enlarged thyroid gland) or thyroid nodules (abnormal growths within the thyroid gland). Your primary care physician or an endocrinologist can treat hypothyroidism with a once-daily prescription of a synthetic thyroid hormone. However, your doctor may refer you to a head and neck surgeon for your thyroid if you have a goiter, hyperthyroidism, or a thyroid nodule.
What is a goiter?
Physicians use the term goiter to describe an enlargement of the thyroid gland. This enlargement can be the result of multiple causes. The most common cause worldwide is iodine deficiency, which affects roughly 30% of the world’s population. However, in the United States, we add iodine to table salt; therefore, an iodine deficient goiter is rarely seen, making most in the US due to other causes. One point that often confuses patients is that goiters are not necessarily associated with abnormalities of thyroid function. A patient can have a very large goiter but at the same time have normal thyroid function. Likewise, a patient may have only a very small goiter but a large degree of hyperthyroidism. Either of these conditions may result in the need for surgical treatment.
Nontoxic goiter or multinodular goiter
A nontoxic goiter is the name given to an enlarged thyroid gland that is not associated with hyperthyroidism. These goiters are often comprised of multiple abnormal nodules that form within the gland, giving it an abnormally enlarged appearance. For this reason, we refer to these goiters as multinodular. Patients often detect the presence of a multinodular goiter or a physician may make an incidental finding during a routine physical examination or x-ray of the neck. Most patients with multinodular goiters do not experience symptoms; therefore, the concern essentially revolves around any possible presence of cancer and any risk of hyperthyroidism. Your doctor can address these concerns with simple tests, such as biopsies that can rule out the presence of cancer and blood tests that can detect the presence of hyperthyroidism.
With a multinodular goiter, some patients may experience symptoms as a direct result of pressure exerted by the enlarged thyroid gland. These compressive symptoms include difficulty breathing or swallowing, hoarseness, or an uncomfortable sense of pressure in the area of the gland itself. If you experience these symptoms, your doctor will refer you to a head and neck surgeon for surgical removal of the enlarged thyroid gland.
Hyperthyroidism and toxic goiters
For some patients, a toxic goiter that is associated with hyperthyroidism is detected in your blood test. If the test shows hyperthyroidism, your doctor can order a special type of x-ray called a nuclear medicine study. This test can help in determining the exact underlying cause of hyperthyroidism. The most common cause of a toxic goiter is a condition called Graves’ disease, which is an autoimmune condition that affects the thyroid gland causing it to become enlarged and overactive. Multinodular goiters can also be toxic. While hyperthyroidism may be brought under control with medications, the drugs can have unpleasant side effects and are therefore not considered appropriate for long-term or definitive management. Another option for treatment in cases of either Graves’ disease or toxic multinodular goiter is radioactive iodine therapy. A radiation oncologist provides this treatment to resolve hyperthyroidism through a nonsurgical modality. Radioiodine therapy does come with its own set of special considerations and potential side effects that can cause it to be a less than satisfactory solution depending on the individual and their medical history. For these reasons, patients with both Graves’ disease and toxic multinodular goiters are often referred to a head and neck surgeon for removal of the thyroid gland to resolve the problem. Your doctor will talk with you to help you determine which course of treatment is best for you.
What is a thyroid nodule?
Thyroid nodules are the most common reason why individuals see a head and neck surgeon. An individual may have only a single nodule (often referred to as a solitary nodule) or they may have multiple nodules within the thyroid gland (often referred to as a multinodular goiter as previously discussed). It is important to understand that nodularity within the thyroid gland is extremely common. Researchers estimate that somewhere between 35 to 50% of individuals have at least one nodule within the thyroid gland. The patient or their health care provider often discovers nodules as a lump or swelling in the lower neck just below the Adam’s apple. Increasingly, thyroid nodules are discovered incidentally (meaning by accident) on imaging studies of the neck or chest, cervical spine, or carotid arteries which were originally obtained for evaluation of unrelated conditions. Thyroid nodules can be large enough to produce compressive symptoms and, in rare instances, can be overactive in their production of thyroid hormone. For the most part, however the overriding clinical concern is the potential presence of thyroid cancer.
Fortunately, most thyroid nodules are benign. Physicians estimate that only 5% of all thyroid nodules are cancerous. Age, sex, family history, and a history of head and neck radiation therapy, all affect the prevalence of both benign thyroid nodularity and thyroid cancer. The presence of thyroid nodularity increases with age. In general, a nodule in a patient under the age of 20 is twice as likely to be malignant and a nodule in a patient over the age of 70 has a fourfold increased risk of malignancy. While nodules are more common in women, the risk of malignancy in men is twice is high.
The initial diagnostic approach typically involves obtaining a thyroid ultrasound and thyroid blood tests ordered by either your primary care physician or an endocrinologist. Thyroid ultrasound is an invaluable tool in determining the size and characteristics of a thyroid nodule. While there are some characteristic features, which may appear on sonography that might suggest an increased risk of malignancy, by far the most important predictor is nodule size. In general, any nodule 1 cm or larger will typically require further investigation in the form of a minor outpatient procedure called a fine needle aspiration (FNA) biopsy. If FNA biopsy is either positive or suspicious for the presence of malignancy, your doctor will recommend thyroid surgery.
See your doctor
Your primary care providers can often diagnose disease of the thyroid gland with a physical examination and routine blood test. While the majority of these conditions can be either safely observed or medically managed, there are subsets of thyroid conditions that require surgery for proper management. The key to a good outcome in all instances is maintaining proper follow-up with your primary care doctor for routine examinations and blood testing.
Author: Daniel R. Blankenship, MD | Columbus, Georgia
Last edited on July 27, 2022