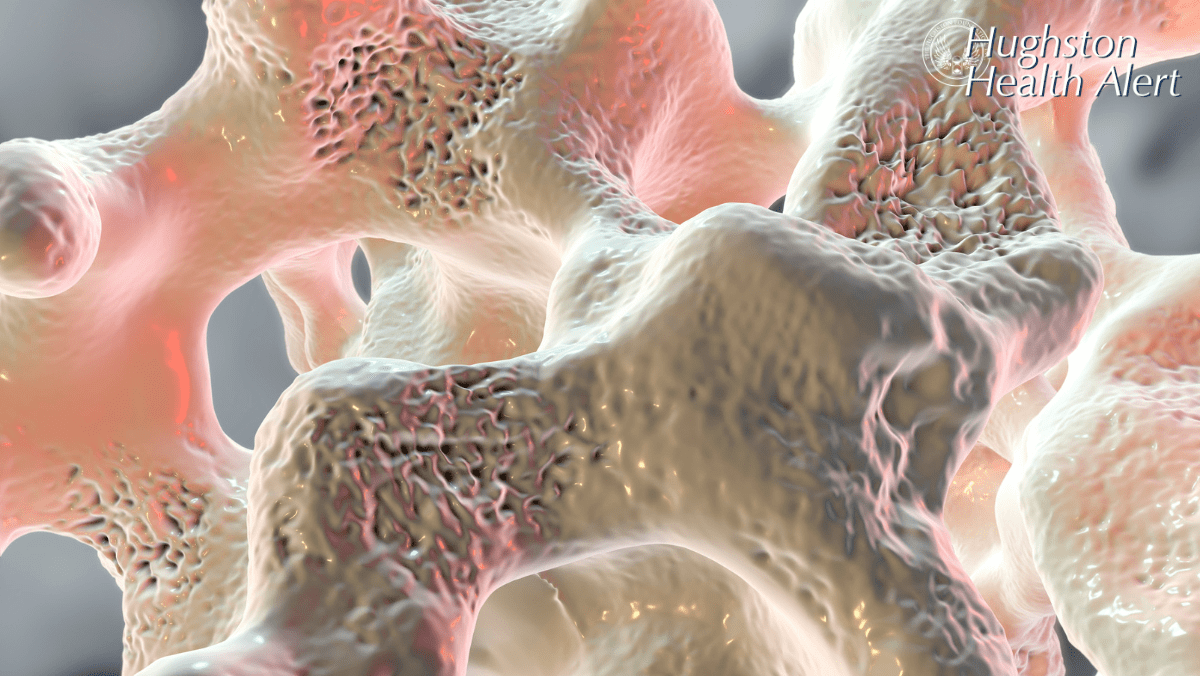
 Have you ever been told you have “weak bones?” Osteoporosis, or poor bone quality, affects millions of people as they age. An estimated 10 million people in the United States have osteoporosis, and women are 4 times more likely to develop osteoporosis than men. However, did you know that osteoporosis is actually not a bone quality problem? Instead, as you grow older, it becomes increasingly more difficult for your body to make enough bone to maintain good bone density and strength. Therefore, as bones become thinner, they are more likely to break. Osteoporosis makes your bones susceptible to fractures, or breaking, which can be very painful, can decrease your ability to enjoy life, and can even increase your risk of serious illness and subsequent death. Don’t worry, physicians have become very good at identifying, diagnosing, and treating osteoporosis.
Have you ever been told you have “weak bones?” Osteoporosis, or poor bone quality, affects millions of people as they age. An estimated 10 million people in the United States have osteoporosis, and women are 4 times more likely to develop osteoporosis than men. However, did you know that osteoporosis is actually not a bone quality problem? Instead, as you grow older, it becomes increasingly more difficult for your body to make enough bone to maintain good bone density and strength. Therefore, as bones become thinner, they are more likely to break. Osteoporosis makes your bones susceptible to fractures, or breaking, which can be very painful, can decrease your ability to enjoy life, and can even increase your risk of serious illness and subsequent death. Don’t worry, physicians have become very good at identifying, diagnosing, and treating osteoporosis.
Causes and risk factors
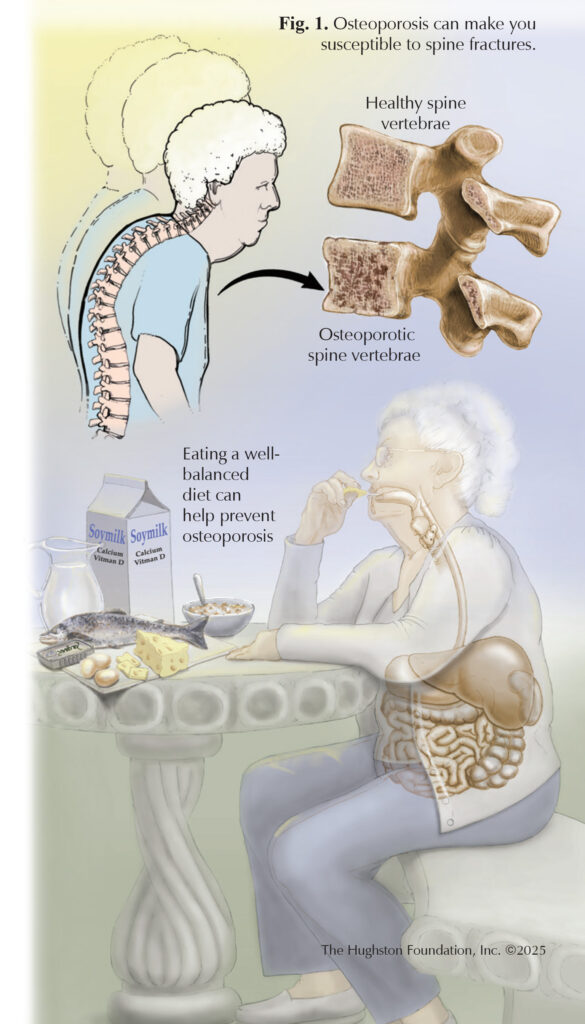
The most common type of osteoporosis is postmenopausal, which occurs most often in women aged 50 to 70, who have a decline in female hormone levels. Osteoporosis can also occur in men or in women older than age 70, but this results from a combination of other factors. These can include lifestyle factors such as poor diet, little exercise, long-term tobacco or heavy alcohol use, as well as medical conditions such as diabetes, kidney disease, thyroid disease, or cancer. You even have a greater risk of developing osteoporosis if your parents had it.
Symptoms
Unfortunately, most people do not realize that they have osteoporosis until they fall and break a bone. The 3 most common types of “fragility” fractures (those due to osteoporosis) are vertebral body (spine), hip joint, and distal radius (wrist) fractures. The majority of fragility fractures occur when falling from a standing height. If you sustain a fall and are unable to bear weight, unable to move your limbs without extreme pain, or have significant swelling, seek immediate medical attention. An orthopaedist can identify and stabilize a fracture and provide immediate management of your injury.
Diagnosis and screening
Physicians can observe osteoporosis or thinning bone on all types of medical imaging, including x-ray, CT scan, or MRI. If there is concern, your doctor may refer you for a Dual Energy X-ray Absorptiometry, or DEXA scan, which is the best imaging study used to diagnose osteoporosis. However, you can also receive an automatic diagnosis of osteoporosis if you sustain any of the 3 fragility fractures. If you have already sustained a fracture of this kind, you should obtain a DEXA scan to help your doctor determine your bone health and if you require treatment to decrease your risk of additional fractures in the future. The U.S. Preventative Services Task Force (USPSTF) recommends that all women who are postmenopausal and older than 65 years of age undergo DEXA scanning for osteoporosis. However, even postmenopausal women younger than 65 years should undergo DEXA scanning if you have risk factors.
Management and prevention
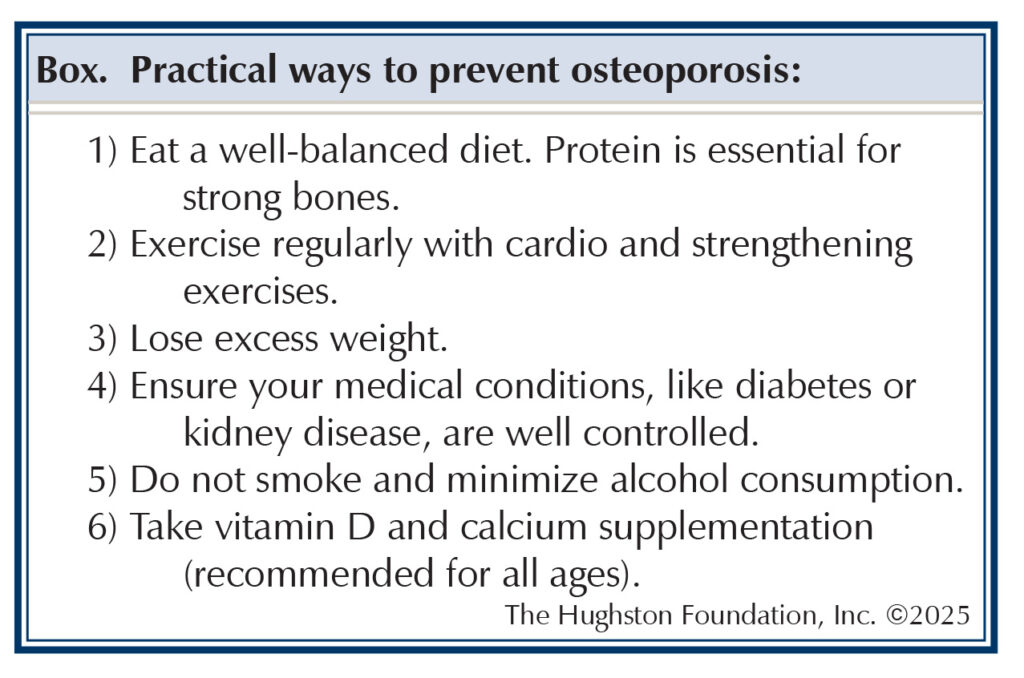
Management of osteoporosis is prevention of osteoporosis.
Treatment
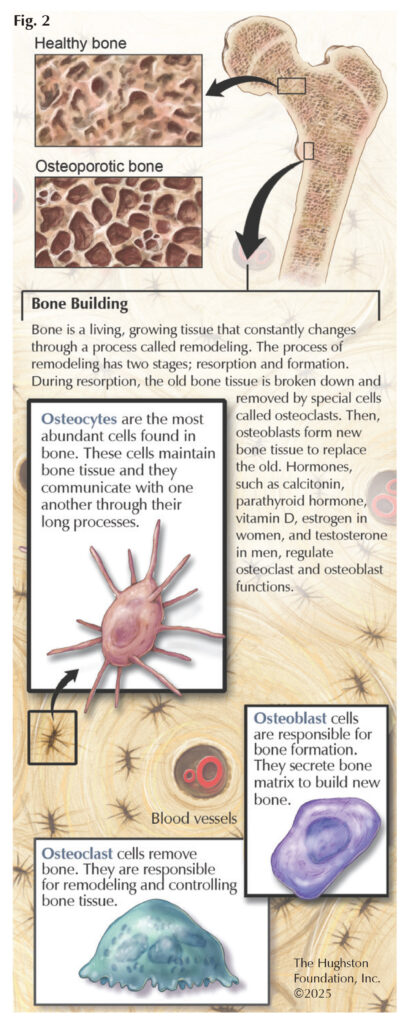
If you are diagnosed with osteoporosis or sustain a fragility fracture, the best treatment is with medications called bisphosphonates, which inhibit osteoclasts (cells that break down bone.) This allows osteoblasts (cells that make bone) to make more bone before it breaks down (Fig. 2). Remember: osteoporosis occurs when the body isn’t able to make enough bone. Additionally, individuals of all ages should take vitamin D and calcium supplements, as it is hard to obtain the full daily requirement from your diet alone.
Outcomes
Of patients with untreated osteoporosis who sustain a fracture, 10% will sustain another fracture within 1 year, 18% within 2 years, and 31% within 5 years. Patients who sustain a vertebral body fracture, have a 30% increase in mortality rate, and these patients also have a 5x higher chance of sustaining a hip fracture.¹ Similarly, hip fractures increase the risk of death by up to 36% within the first year after fracture² and multiply the risk of a second hip fracture by 10 times.
With bisphosphonate therapy alone, studies have shown a 14% reduction in mortality rate following vertebral fractures.³ Most importantly, the longer the patient is on the treatment, the greater the risk reduction. Similarly, the cumulative risk of hip, spine, and wrist fractures can decrease by as much as 50%. Likewise, with appropriate calcium and vitamin D supplementation, you can reduce your fracture risk 34% and 30%, respectively.4
You’re not alone
Osteoporosis affects millions of people worldwide, so you’re not alone! Know your risk factors and seek appropriate treatment to avoid fracture injuries, which can increase your risk of future fractures and fracture-related mortality. The key to treatment is prevention. Physicians recommend lifestyle changes that include a balanced diet and exercise along with vitamin D and calcium supplementation. If you do develop osteoporosis, there are treatment plans that are effective in reducing your fracture risk.
Above all, ask your primary care doctor or an orthopaedic provider about your risk factors and treatment options to maximize your bone health and improve your quality of life.
Author: Jon Christopher Gibbs, Jr, MD | Columbus, Georgia
Resources
- Balasubramanian A, Zhang J, Chen, L. et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019;30:79–92.
- Abrahamsen B, van Staa T, Ariely R, et al. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633-1650.
- Tai TW, Tsai YL, Shih CA, et al. Refracture risk and all-cause mortality after vertebral fragility fractures: Anti-osteoporotic medications matter. J Formos Med Assoc. 2023;122 Suppl 1:S65-S73.
- Edgington, J. Osteopenia & Osteoporosis. Orthobullets. 28 March 2025. www.orthobullets.com/basic-science/9032/osteopenia-and-osteoporosis.
Last edited on October 17, 2025