
If you run your hand down your neck and back, the thin bony projections you feel are the spinous process. A fracture of the spinous process of a lower cervical (neck) or upper thoracic (middle back) vertebra is sometimes called clayshoveler’s fracture because the injury occurs primarily in workers who shovel heavy loads for long periods. Doctors originally coined the term in 1940 to describe isolated spinous process fractures occurring from C6 to T3. Once a common occupational injury during the 20th century, it has become relatively rare since the introduction of earth-moving machinery. Today, spine orthopaedists diagnose this fracture pattern in a variety of patients, including football players, power-lifters, golfers, skiers, and trauma patients.
 Anatomy
Anatomy
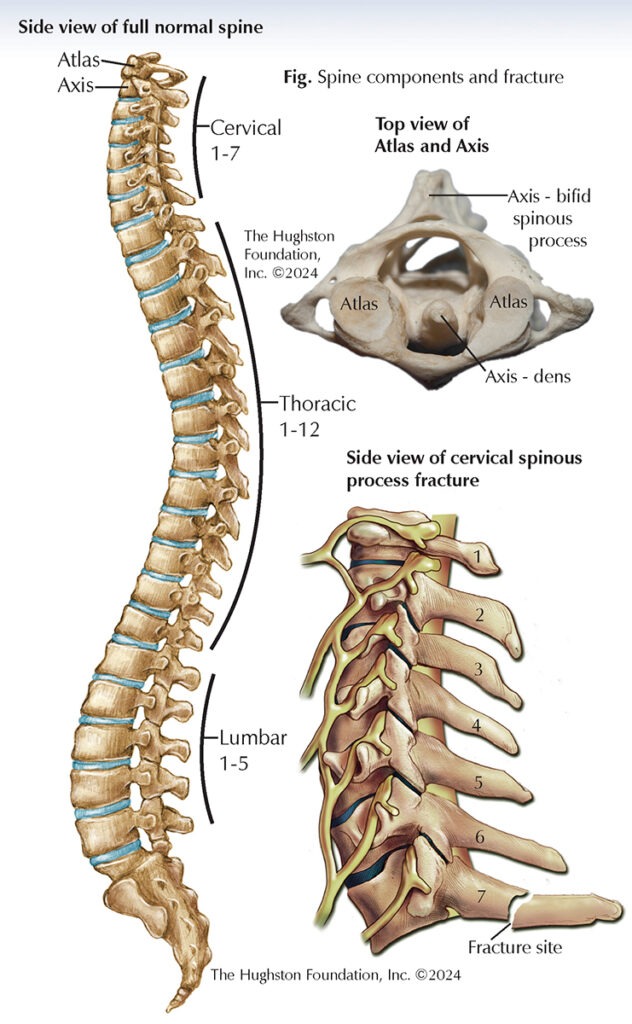
The cervical spine is made up of 7 vertebrae, which are numbered C1 through C7. The first cervical vertebra C1, the atlas, has no vertebral body and no spinous process. C1 is a ring-shaped vertebra that supports the head and sits on top of the second cervical vertebra, C2, which is the axis. The axis has a bony projection called the dens that fits into the ring of the atlas and allows for head rotation. The remaining five cervical vertebrae, C3 through C7, are similar in structure and function (Fig). They have small bony projections called spinous processes that extend out from the back of each vertebra. These processes serve as attachment points for muscles and ligaments that control the movement of your head and neck. The spinous processes of C2 to C6 vertebrae are bifid (split into 2). The C7 vertebra, which is the most common fracture site, has a much larger and singular spinous process, known as the vertebra prominens, and is similar to those of the thoracic vertebra.
Type of injury
Typically, this type of injury is a stress-type avulsion (ripping or tearing away) fracture involving the spinous processes of the lower cervical or upper thoracic vertebra. Often, the injury occurs when the end of the spinous process fractures either by physical impact or from the muscle pulling so hard that it breaks the bone. The bone can fracture and remain in place or it can displace and tear off part of the spinous process. The fracture usually occurs midway between the spinous tip and lamina and it does not cause any structural, functional, or neurological impairments. Although C7 and T1 are the most commonly involved spinal levels, an avulsion fracture can occur at any lower cervical or upper thoracic level, as solitary or multiple fractures.
Symptoms
The first symptom is immediate pain between the shoulder blades or base of the neck with reduced head or neck range of motion. Patients often describe a burning or stabbing pain, muscle tightness, and sharp pain that increases with repeated activity and movement. The area of the fracture and nearby muscles are often tender. If only the spinous process is injured, you will not have any neurologic symptoms, such as tingling or numbness. You may lose head, neck, and shoulder motion since movement can cause the muscles to pull directly on the site of injury and limit your desire to move.
Diagnosis
An orthopaedic spine doctor will perform a physical exam and order x-rays or magnetic resonance imaging (MRI, a scan that shows bones, muscles, tendons, and ligaments). During the physical exam, the doctor will look for localized swelling, tenderness, and crepitus (a grating sound or sensation produced during movement of the fractured bone). The doctor will also complete a neurovascular exam. Your doctor may confirm your diagnosis using x-rays; however, if the fracture is suspected but no evidence of injury is found on radiographs, MRI images can show the soft-tissue avulsion of the spinous process.
Treatment
The treatment is often conservative, involving rest, immobilization using a collar, pain medication, and activity modification for a period of 4 to 6 weeks. The orthopaedist may recommend surgical treatment if there is nonunion (failure to heal) of the displaced fracture. With nonoperative treatment, patients can often return to sports by 4 months after injury. For a spinous process fracture, data shows high union rates and excellent clinical outcomes.
Author: Brittney L. Lambie, MD, FAAOS | Lake Nona, FL
Last edited on January 30, 2025