
In the 16th century, King Charles IX experienced endless pain and contractures after he underwent a surgical procedure. Ambroise Pare (known as the father of modern surgery) recorded the King’s treatment, which is thought to be the earliest documented description of complex regional pain syndrome (CRPS).1 Formerly known as reflex sympathetic dystrophy (disorder of the sympathetic nervous system) and causalgia (affecting a peripheral nerve), it was not until 1994 that the International Association for the Study of Pain renamed these pain syndromes as CRPS Type 1 and CRPS Type 2, respectively.2
Who does it affect?
CRPS is a rare and debilitating disease that affects less than 2% of individuals in the United States. Race is not a factor, but females are affected more than males, and the peak age of patients is 40 to 49 years. Additionally, the upper extremities are affected more often than the lower extremities.2
What are the symptoms?
CRPS patients experience chronic pain with sensory and motor symptoms in their limbs. With CRPS, there is usually a damaging or inciting event that causes injury, such as trauma, surgery, or a period of immobilization.
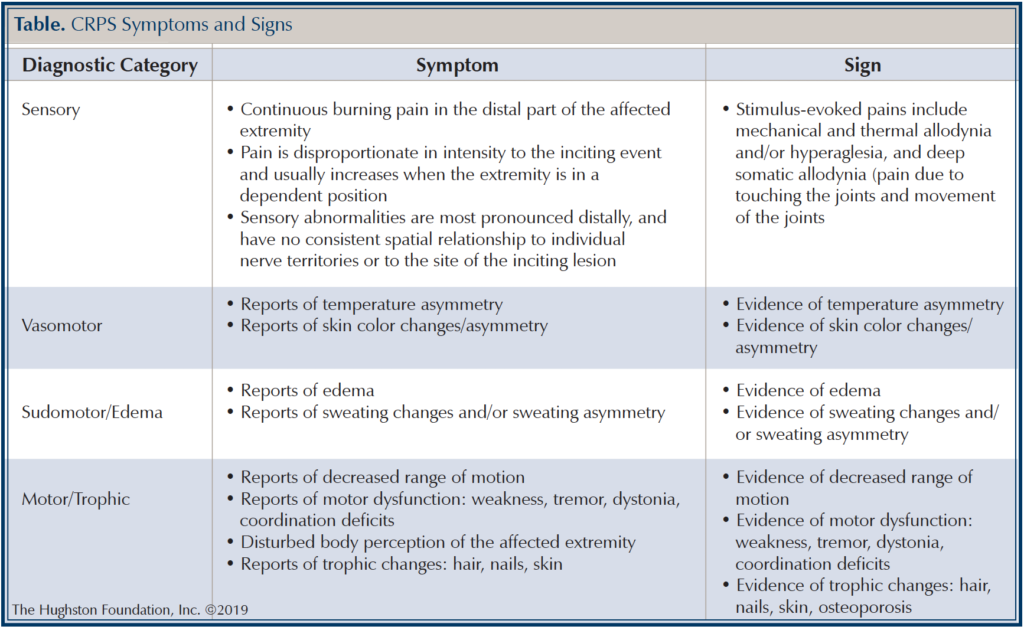
The difference between the 2 types is that Type 1 does not have a distinctive injury to a nerve, whereas patients with CRPS Type 2 have a known nerve injury. To help diagnose CRPS, the Budapest criteria (Table) were established in 2003. In patients who have continuing pain that is disproportionate to any inciting event, they must report 1 symptom in 3 of the 4 following categories: sensory, motor/trophic, vasomotor, sudomotor/edema.1 The patient must also display at least 1 sign at the time of evaluation in 2 or more of the categories. Lastly, there cannot be another condition that would account for the degree of pain and dysfunction that the patient is experiencing.
There are 3 stages of CRPS: acute, subacute, and chronic.2 The acute stage lasts 3 months. During this stage patients usually have a burning type pain, swelling, skin redness, increased sweating, and decreased range of motion. After 3 months, the patient enters the subacute stage. During this stage patients have continued severe pain, swelling, skin dryness, and paleness or bluish coloration of the skin. After 12 months, the patient progresses to the chronic stage that can last for multiple years or even become permanent. In the chronic stage, the patient’s pain is variable and can continue to be severe or it may subside. The patient’s skin is dry, shiny, and cool to the touch. Also, since the patient has not been using their extremity, the underlying bones can develop osteoporosis (a disease that weakens bones).3
How is CRPS diagnosed?
There are no specific laboratory studies that make the diagnosis of CRPS; however, it is imperative to obtain laboratory studies so that other disease or disorders can be excluded as the cause of the patient’s symptoms.2 Imaging studies that are useful include radiographs (x-rays) and bone scans (an imaging test that helps diagnose bone disease). Since CRPS Type 2 involves a known nerve injury, a nerve conduction study can provide useful information as well.4
How is CRPS treated?
The best treatment for CRPS is to use a multidisciplinary team approach to alleviate the patient’s pain and help the patient regain function of the extremity.1 For example, a pain specialist helps control the patient’s pain using medications and injections. A surgeon is needed for procedures that help control pain and regain extremity function. A primary care physician can help with the patient’s pain control as well as helping with other symptoms, such as swelling, inflammation, and depression. Physical therapists and occupational therapists are critical in improving the functional outcome of the affected extremity with range of motion exercises and other modalities.5
Getting help
CRPS results in debilitating pain and significant loss of function in the extremities. In order to improve patient outcomes, CRPS should be recognized early on and treatment initiated as soon as possible. Pain specialists, surgeons, physical therapists, and other healthcare providers each play a role in helping the patient get back to a normal routine. If you are experiencing chronic pain, talk to your doctor, getting help is the first step toward a pain-free life.
Author: Mudassar A. Khan, DO | Columbus, Georgia
References
1. Sebastin SJ. Complex regional pain syndrome. Indian Journal of Plastic Surgery. 2011;44( 2):298-307.
2. Goh EL, Chidambaram S, Ma D. Complex regional pain syndrome: A recent update. Burns & Trauma. 2017;5(1):ecollection. doi:10.1186/s41038-016-0066-4.
3. Baron R, Binder A. Complex Regional Pain Syndromes. Baron R, Binder A, Pappagallo M, editors. In: The Neurological Basis of Pain. New York, NY: McGraw-Hill; 2005:359-378.
4. Harden RN, Oaklander AL, Burton AW, et al. Complex regional pain syndrome: Practical diagnostic and treatment guidelines, 4th ed. Pain Medicine. 2013;14(2):180-229.
5. Stengel M, Binder A, Baron R. Updates on the diagnosis and management of complex regional pain syndrome. Advance Pain Management. 2007;1(3):96-104.
Last edited on October 18, 2021